Many people who carry extra weight on their bodies have stories to tell about problematic medical care. Maybe a medical issue was overlooked because of their weight. Perhaps a doctor prescribed losing weight as a solution to an issue that had nothing to do with being fat.
In our society, fat is looked upon as a health hazard at best and a character flaw at worst. While evidence does point to obesity being a health risk factor, judgments about other people’s extra pounds go far beyond concerns over health. Companies make billions of dollars off of perpetuating society’s obsession with thinness, from diet pills to weight loss programs to plastic surgery, and fat jokes seem to be the final frontier of socially acceptable cruelty and marginalization.
This obsession with the size of people’s bodies has consequences. People have no problem sounding off about health problems associated with obesity, but rarely do we hear people preach about about health consequences of the fear of obesity. Anorexia and bulimia come to mind, but there are also more nuanced tales of people facing medical neglect and abuse from others due to a pervasive fear of fatness. We’re talking about illness and death in babies and children, all because of fatphobia.
RELATED: These 3 stories show how we’re subconsciously teaching children to be fatphobic.
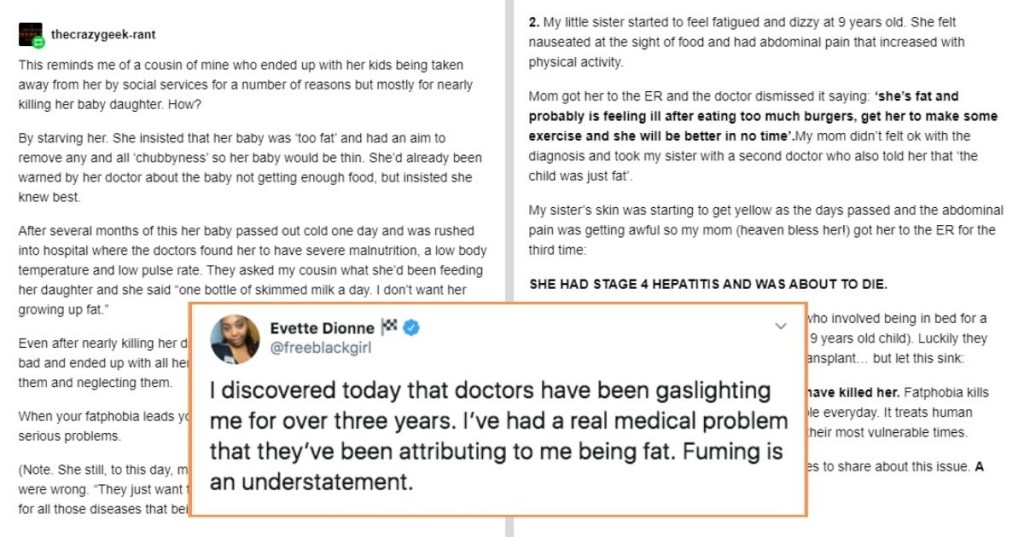
In a post on Facebook shared by Dadmin, a series of screenshots of Reddit stories illustrating how fatphobia can lead to dire health problems. Sometimes those problems are even exacerbated by healthcare workers themselves.
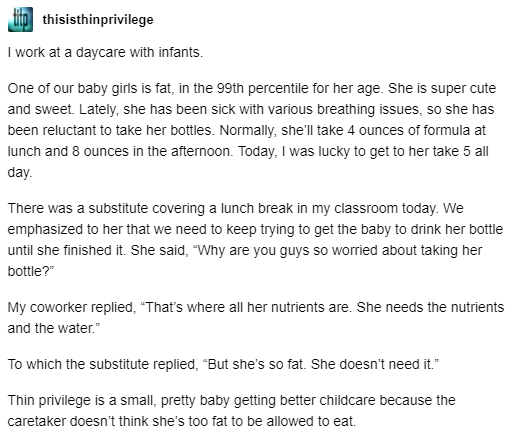
One person told the story of a substitute at a daycare where she worked questioning why a large baby needed to take a bottle. A coworker replied, “That’s where all her nutrients are. She needs the nutrients and the water.” The substitute replied, “But she’s so fat. She doesn’t need it.” All babies need to eat regularly, and all babies’s bodies are different. (For example, my own babies were super roly-poly, and all they had was breastmilk their first 10 months or so. My best friend’s baby, also exclusively breastfeed, ate far more frequently than mine and was super skinny.)
As the poster pointed out, “Thin privilege is a small, pretty baby getting better childcare because the caretaker doesn’t think she’s too fat to be allowed to eat.”
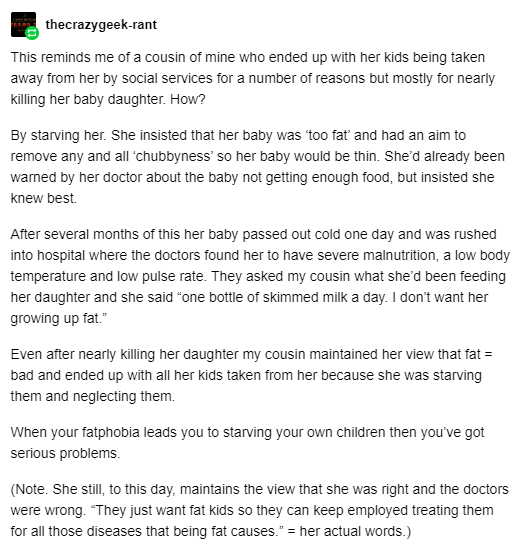
Another person wrote about their cousin who had her kids taken away because she was starving her baby. Worried about her infant becoming “too fat,” she only fed her one bottle of skim milk a day. “I don’t want her growing up fat,” she said. Even after having her kids removed for medical neglect, she still maintained that the doctors were wrong and she was right. According to the post, she said, “They just want fat kids so they can keep employed treating them for all those diseases that being fat causes.”
Other people chimed in with similar stories of babies being starved or evaluated as overweight.
“A parent brought in their six month old baby who was having breathing issues and kept getting sick,” one person wrote. “The parent was asked if the baby was eating regularly and the parents straight up told the doctor that they only feed the baby once a day…They even had the nerve to say because they didn’t want the baby to get fat. People like this are real. They would rather have a dead baby than a fat one.”
Another shared the story of their exclusively breastfed 10-month-old being in the 99th percentile and the nurse saying, “He is at risk for obesity. You may want to keep an eye on that.” She said later on, this same child measured off the charts but the doctor said at least he was in proportion. Because they can’t control their “weight talk,” which research shows is potentially harmful to children, this mother said she no longer allows doctors to weigh her kids unless it’s medically necessary. (And it sometimes is. Medication dosages are often determined by height and weight, for example.)

Another person wrote about how her mother had her dieting with her from the time she was 11, worried she was going to “get huge.” She fed her less than 600 calories per day and grounded her when she found out her friends were bringing her lunches. She ended up in the ER and has struggled since with anorexia. “Please don’t starve your fucking children,” she wrote.
RELATED: A viral and heartbreaking hashtag proves body-shaming starts early for women.
As another user wrote, “Fatphobia is real and it kills.”

Sometimes healthcare providers think every health issue is weight-related, which can result in misdiagnosis.
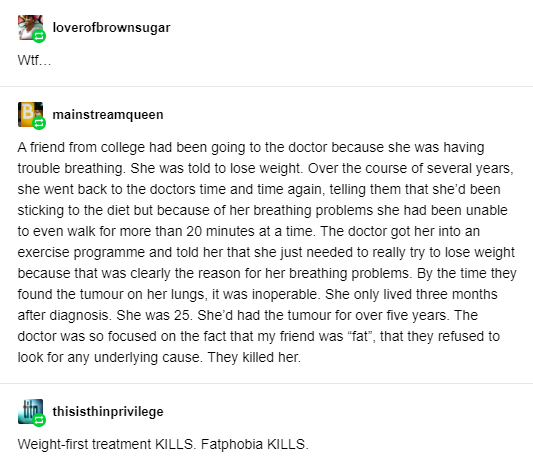
One person shared a story of a college friend who had been having trouble breathing. The doctor told her to lose weight. Time and again over several years, she returned to the doctor with the same breathing problem, telling them she was dieting but couldn’t exercise because of the breathing issue. It turned out she had a tumor on her lungs that wasn’t caught. She died at age 25, three months after it was finally diagnosed.
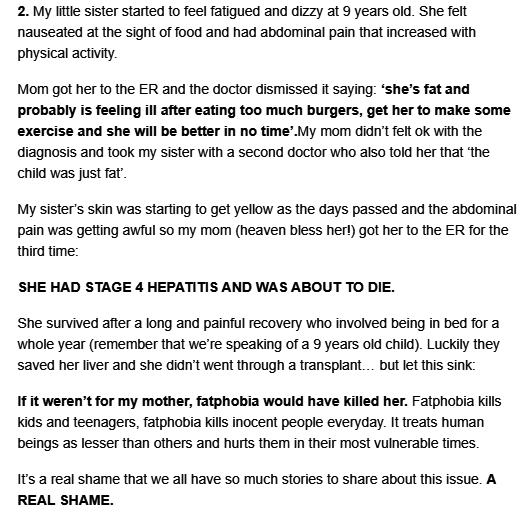
Yet another user shared a story of her little sister feeling fatigued and dizzy, getting nauseated at the sight of food, and suffering from abdominal pain at nine years old. The ER doctor dismissed it saying she was fat and probably just ate too many burgers. Her mom questioned the diagnosis and took her to another doctor who also told her that the girl was “just fat.”
The pain got worse, the girl’s skin began to yellow. A third ER visit revealed she had life-threatening hepatitis, which took a year to recover from. “If it weren’t for my mother, fatphobia would have killed her,” the person wrote.
Clearly, some of these stories are extreme, and one must take Reddit stories with a grain of skepticism. But stories like this abound across social media.
And there is more than just anecdotal evidence that prejudice against fat people can cause real medical harm.
A 2015 Lancet study found that doctors take less time with obese patients and are more reluctant to screen them for other health issues. It also found that healthcare workers tend to stereotype obese people as less likely to follow medical advice and stick to medications.
A 2017 review of research from the American Psychological Association also found that medical discrimination based on people’s size is a real issue, and obese patients are more likely to have undiagnosed medical issues:
“In one study of over 300 autopsy reports, obese patients were 1.65 times more likely than others to have significant undiagnosed medical conditions (e.g., endocarditis, ischemic bowel disease or lung carcinoma), indicating misdiagnosis or inadequate access to health care.”
When societal judgments on weight start affecting people’s medical care, we have a problem. And it can’t only be fat people battling the issue—it’s up to all of us to fight size bias and tackle the myriad messages we see every day that fat people are less than.
As one Reddit user said, “I’d really like my thin followers to reblog this if you can. Fat people are already here for each other. We need you guys to help us out too. This is something I never see anyone actually talking about in-depth, and it’s disappointing.”
Let’s talk about it now, and do what we can to eliminate fatphobia before it does more harm than it already has.