When we talk about the coronavirus pandemic, we often talk about numbers. How many cases. How many deaths. How many recoveries.
But the true impact of the virus goes far beyond those statistics. We’ve seen this in harrowing stories from medical workers on the front line and from people who have made it out of hospitalization.
While there’s so much we still don’t know about COVID-19, as more people recover we get more stories of what the disease can do. We know that it can infect people with no symptoms. We know that it can kill. What we see less often is what it can do to those who get sick but don’t die.
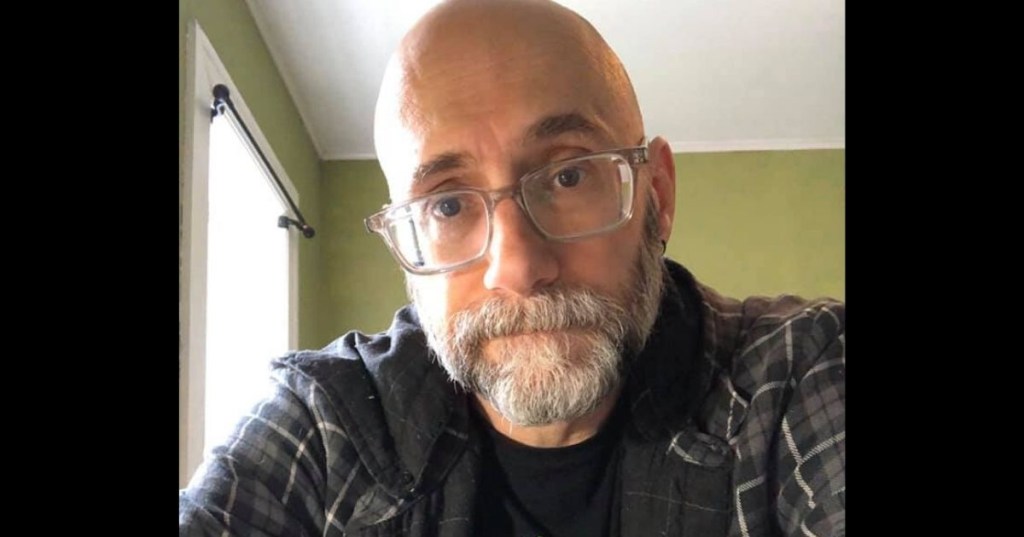
Barry Mangione is a pediatric physical therapist who contracted the virus just over a month ago. As a healthy 50-year-old with no underlying health conditions, one might assume he’d weather the illness without too much trouble. But as he described in a Facebook post, this isn’t a “get it and get over it” kind of disease for many people who have officially recovered.
Mangione wrote:
COVID19 is a continuum.
I want to hopefully shed some light amid the confusion. There is a continuum of COVID19 in between ‘you die’ and ‘you get over it and return to normal.’ Today is day 31 for me. I tested negative on day 27. Yesterday out of nowhere, I was hit with crippling fatigue and chills. My cough is almost gone, and I’ve been fever-free for two weeks, but when it comes to COVID19, testing negative doesn’t mean it’s over. For all who talk about wanting it to spread among the healthy to encourage ‘herd immunity,’ let me ask you: if you get sick with COVID19, how do you know how sick you’ll get? I’m a healthy 50 year old with no underlying medical conditions. Those of you who know me know that I am passionately devoted to developing and maintaining mental, physical, and spiritual health.
I’m a pediatric physical therapist. I work in homecare with infants and toddlers. Prior to COVID19, I would travel to people’s homes and work with up to ten children a day for 30 minutes each. Prior to COVID19, I struggled with insomnia, but I could still get up after a nearly sleepless night and rock my day job. Now, I can get a full night’s sleep and be wiped out after doing a couple of telehealth sessions with kids via Zoom. Let me repeat that. I used to travel to different homes, play with up to ten kids a day, and now some days I’m exhausted after sitting at a desk and talking to parents via a screen.
I talk to other COVID19 survivors who still experience symptoms after 30, even 40 days, symptoms like kidney pain, fevers, coughing, fatigue, shortness of breath, headaches, circulation problems, loss of smell, loss of taste, body aches, rashes, back pain…
This is not an all-or-nothing virus. It’s not ‘you die’ or ‘you don’t die.’ When we see the numbers of people who’ve ‘recovered from COVID19’ posted to illustrate how it’s not that bad, those numbers don’t take the lingering health issues and symptoms into account.
Please think about this when you question social distancing. Please think about this when you question wearing a mask in public. Ask yourself, ‘Can I be sick for over a month or more? Can I deal with the uncertainty of when or if this sickness will go away if I get it?’
I’m not looking for sympathy or trying to scare anyone, and I don’t want to diminish the memories of those who’ve died or the pain felt by their loved ones. I grieve for them all. What I hope I’m doing is giving you another tool in addition to gloves, masks, and social distancing to keep yourselves, your loved ones, and all of us safe and healthy: knowledge that this is real, knowledge that we don’t know enough about it yet, and that the continuum of COVID19 is more complicated than dead versus ‘recovered.’
Please stay safe, my friends.
Mangione’s story is important not just for our understanding of what the virus can look like for those who have “recovered,” but also for our understanding of what it might look like if we were to shoot for herd immunity. Despite the much higher death count that would result, it seems that more and more people are leaning toward trying to achieve herd immunity through letting 60% to 80% of the population get infected with the virus instead of waiting a year or more for a vaccine. Some are surprisingly willing to accept more deaths in exchange for saving the economy—but would it actually save the economy? Imagine a large portion of the population getting sick in the way Mangione describes. What would that do to the economy, when millions of people are too sick to work for a month or more? (Though some people will fly through infection without any symptoms, we don’t have proof yet that asymptomatic cases will outnumber those who actually do fall ill.)
Until we have a reliable treatment or vaccine, we’re going to have to get used to the idea of life not going back to normal. We’re either locked down with fewer illnesses and deaths and a choked-off economy, or we’re dealing with millions sick and dying and still end up in an economic crisis.
Because we don’t yet know the full impact of the virus, and there’s no way to predict how it will affect an individual or how many people they might infect if they get it, health experts are not recommending letting the virus run its course through society. It’s not as simple as “Eh, I’m not old or immunocompromised, so I’m not worried.” Getting sick and getting over it isn’t how this is playing out for many people.
As we continue learning more, keep yourself and your community safe and well by continuing to practice social distancing and good hygiene even as things start to “open up.” As frustrating as it is, we’re not anywhere near out of the woods with this virus.