With protests around the country over pandemic lockdowns, it’s clear that many Americans are frustrated—and understandably so. We’re in a frustrating situation, where leaders and public health officials have to make impossible decisions based on constantly changing data, with terrible consequences resulting from every choice.
But some folks seem to be a bit unclear on exactly what these lockdowns have been preventing. In areas that haven’t been hard hit, the measures feel like an overreaction. That’s why we need to be reminded of the real, dire human toll this virus will take if allowed to spread. And not just in numbers, which are too easy to dismiss, but in stories that describe the reality of what can happen anywhere the virus is allowed to take hold.
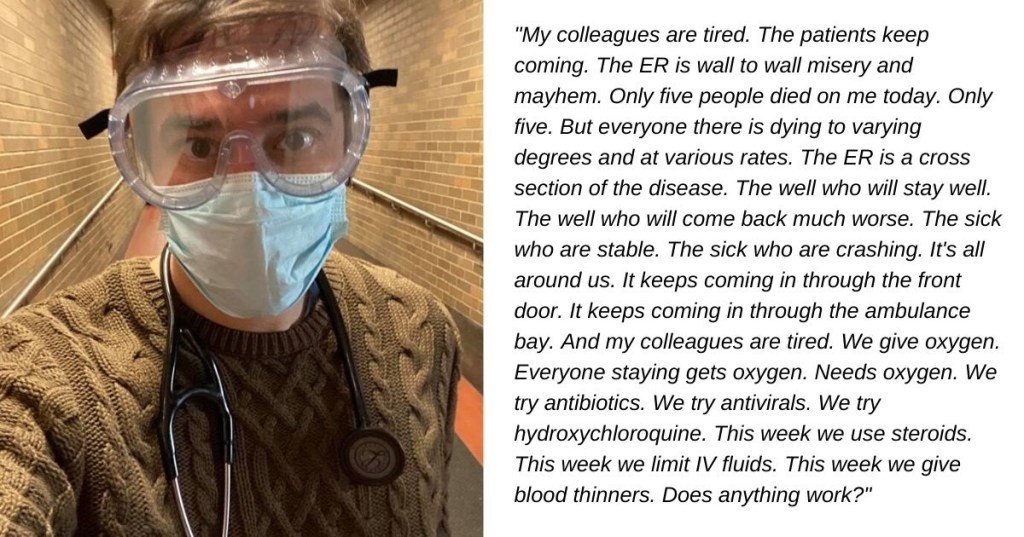
Jason Hill, an ER doctor at New York Presbyterian Hospital in New York City, shared some of his personal journal entries during the peak of New York’s outbreak. They offer a painful but beautifully crafted window into why we’ve been locking down and must continue to do what it takes to keep the spread to a minimum.
Dr. Hill wrote on Facebook on April 15:
“Thanks for all the bday wishes. Several people have asked me about what it’s been like in the ER with Covid. I’d done some journaling the last couple weeks. As I turn forty this is how my head, heart, and soul have been occupied.
Covid at 40.
The eyes stay with you. In peace time most of those we intubate are chronically ill, or profoundly confused, or unconscious and unaware of the world around them. Covid has changed the equation. Most of my patients now remain awake and alert until the end. These days the ER is permeated with frank conversations about death and dying and what a chance to live entails. It is a hard thing to tell a healthy and functional person who felt fine and well six days ago they may be dead in a day or two and humbly ask how aggressive they want us to be. A chance to live comes with the risk of dependence on life support and pain. The alternative is the guarantee of an imminent but peaceful death. I have never had more harrowing, more frequent, more brutally honest, more meaningful, more exhausting conversations in my life. Complete strangers open up to you in profound ways during such times and you can only hope both your expertise and your humanity serve them well. And the eyes stay with you.
For those I intubate, those who choose intubation, I often find myself having a final stare. After all the words are spoken, the decisions made, the medications drawn, the bed positioned, the tubes and drips and ventilators readied, there is a final stare. It is a stare of intention. It is a moment of humanity. It is a shared space, a hallowed space, the final moment of someone’s awareness, possibly forever. It is a space where fear and hope mingle, where autonomy fades into trust, uncertainty into acceptance, and all they have left is placed firmly in your gloved hands. It’s brief, and you’re busy, and time is essential, but you find a few seconds to share this final breath. That stare lasts a moment. That stare lasts a lifetime. And the eyes stay with you.
I see them often in my mind, and although haunting I am glad to keep them with me. I warm my hands on the raw humanity inherent in such moments and they empower me to carry on. For carry on we must because the room is full of agony and sickness and fear that must be attended to quickly and humanely.
//
I am asleep before a long night shift. I awake to the sound of cheers and yells. To hooting and hollering. To the clanging of cow bells and the banging of drums. They yell and shout and scream to honor us. They shout from rooftops and ground floors and all the windows and balconies in between. I am asleep before a long night shift. It wakes me up. I am scared shitless. I think the building is on fire. I run around panicked and confused for several minutes. Why do the fire sirens sound like drums and cowbells? Do I even have a fire escape?? WTF is going on?? Oh. Ohhhhhhh. Ok. I get it now. My heart is still racing, but now I’m grinning. Thanks. I feel grateful…mostly.
//
Oxygen Rounds is a new term we have become all too familiar with. I have a hospital full of medications. Antibiotics and anti-virals and sedatives and vasopressors and steroids and opiates. But the only truly effective medicine we have is Oxygen. We blow it at high flow rates into people’s mouths and nostrils, a crutch to help the lungs that are struggling and staggering. And it’s in a shorter supply than I’d like. It flows forever from spickets on the walls, but we have many times more patients than spickets and even fewer rooms so an ever increasing number of patients on stretchers line hallways further and further from the spickets on the walls. We place portable tanks next to stretchers, but the tanks run out and we can’t refill them fast enough. Once per hour, sometimes twice, I walk the halls, hunting for gauges approaching empty and hoping the cabinet holds a replacement. Invariably I find empty ones and hope it hasn’t been empty long. Invariably someone is turning blue. It’s no one’s fault. it’s everyone’s fault. it’s Covid’s fault. And there just aren’t enough eyes and hands to keep up. I mutter a promise to check three times next hour. I pull a step ladder from the utility closet and string plastic connecters end to end to end threading them from wall spickets through corrugated ceiling tiles to drop down above patients’ heads in the hallway so they aren’t reliant on a tank. It’s hard to tell which knob goes to who, but at least it doesn’t run out. It’s a strange time when a step ladder becomes a more useful tool than a stethoscope.
//
I admitted four of my colleagues today. Four of them. They had the usual symptoms. A week or so of cough and chills, fever and body aches, fatigue and loss of smell. They stayed at home and took Tylenol and sipped chicken soup and wondered which patient they had gotten it from. They stayed inside and washed their hands and waited to feel better. But better never came. The cough worsened, they had trouble walking around their home without getting winded, and they knew all too well what that meant, so they came, each of them, not knowing the others were doing the same. I’m in a room with four chairs housing four colleagues with oxygen flowing into their four noses. I’m used to seeing strangers, people I care about because they’re human, but a stranger still. I can maintain a detached distance. This is different. These are my friends and colleagues. These are the people I suit up with and go to battle beside. This is my team. I’ve had harrowing experiences beside them for years. They keep me sane and effective and capable. Together we’ve saved lives and lost lives and everything in between. But now they are on the other side of the curtain. Their coughs hurt my ears more, their fear becomes my fear, I check on the them to the point of harassment, can’t help it, can’t fix it, they’re on a path I can’t cure, can only support through. Can only stand beside them and hope. They try to reassure me, a strange role reversal that belies their strength. I well up with a deep respect. I well up with tears. The front line really feels like the front today.
//
The makers are my favorite people this week. Several days ago I intubated without a face shield. It was three in the morning and we had run out. There were simply more intubations than face shields and we had burned through the stash. But a patient came in and was suffocating in their own lungs and needed a breathing tube, so they got one, and they got one from me, and I did not have the proper armor. Today I stand in a room with hundreds and hundreds of face shields. They are pulled hot off the 3D printers like newspapers off a press. They are arranged on tables by volunteers who add elastic bands and attach shields to complete the ensemble. In the background the gentle hum of a dozen printers working around the clock is an echo of the thousands of engineers and designers, seamstresses and manufacturers, cooks and delivery workers and writers all contributing to the cause. Each shield is a person protected. Each volunteer is a soldier in the fight. I feel less alone.
//
Oxygen means something different in this new reality. In peace time an oxygen level below 95% is bad. An oxygen level below 95% on a non-rebreather face mask is terrifying. That’s a no-brainer. That gets fixed quickly or that gets intubated. Everything is different now. We hang facemasks of oxygen on people with 85-90% saturations for days. They are on the edge of the cliff with one foot dangling and there they stay. Will they inevitably fall off? Are we helping or merely delaying? No one knows. Ventilators are in short supply, ICU beds are full, and ICU docs are tired. We’re all tired. So we temporize, hoping a few will sneak by and not get intubated. Hoping someone doesn’t fall off the cliff when we aren’t looking. The monitors don’t help. They are all beeping and blaring all the time from every direction. The background music of a pandemic. They only tell us what we know, everyone is sick. Only our eyes and experience can help us now. I take another lap around the ER to check the cliffsides.
//
I’m baking a mask tonight. My single use N95 has been on my face for days. The backs of my ears are raw from the rubbing of its straps and my nostrils are filled with the scent of fibers mixed with my coffee flavored breath. My mask bakes and bakes, sterilizing it and killing any viral hitchhikers that attached themselves today. I wish I could do the same for someone’s lungs. It comes out warm and toasty and clean. It comes out safe. I set it on the windowsill to cool, like an apple pie from easier days. Worst desert ever.
//
All hands were on deck today. Elective surgeries have been cancelled and the surgeons and anesthesiologists and neurologists and orthopedists and urologists and rehab specialists and pediatricians have been deputized as ER and ICU docs. Urology attendings and shoulder surgeons are rounding with ICU teams, adjusting ventillators, and drawing blood gases. Pediatricians are seeing adult patients and monitoring oxygen levels. Outpatient docs are working in tents in front of the ER to decompress volume. General surgeons are going from room to room to room putting in Central lines and Arterial lines on our sickest patients. Anesthesiologists are running in to intubate. It remains busy. It remains overrun with sickness and suffering. But today we have more help. Today we have reinforcements. Today we feel like one big army devoted to one fight. Today it feels like maybe, just maybe, we can keep up.
//
Es El Fin. Today I’m a palliative care doc. This man is not doing well. This man needs intubation to survive. He’s 67 and only speaks Spanish. He’s healthy. He’s dying. His oxygen is very low. His respiratory rate is very high. He’s getting tired. He’s suffocating in his own body. He needs to be intubated. He doesn’t want to be intubated. He doesn’t want to be on a machine. We ask if we can help call his family to say goodbye. He looks at us puzzled, somehow still not fully understanding. Esta Muriendo senior. Es el fin. This is the end. He gets it. He’s stoic despite the tears. He’s strong. If this disease attacked character instead of lungs he would have a fighting chance. We set up a video call with his family. He says goodbye. They say they love him in a dozen different ways. He touches the screen. A digital hand hold in a pandemic age. We make him comfortable. He’s still drowning but he can’t feel it. He says thank you before his eyes close. I can’t help but wonder if he would have survived had he been intubated. The odds say no. The sense of defeat within me screams maybe. I try to remind myself this is what he wanted. That this is for the best. I quickly forget.
//
I give out more juice and blankets than I ever have. In peace time the ER is busy, always busy, but most people are not dying. Very few are dying, and even fewer are acutely and actively dying. The scourge of Covid has rewritten those rules. Everyone in the ER tonight is too sick to go home. Many are dying. Many will never leave the hospital. Many will never have a meal or a juice box again. In peace times I often can’t be bothered to bring someone juice. It’s not a priority. Tonight anyone asking gets juice. Even those not asking get juice. Often it’s the only comfort I can provide. A small ease of suffering. A brief distraction from the fear. It may be the last juice they ever drink. Some nights it’s the best medicine I have.
//
We had a patient tonight that impaled her hand with a crochet needle. Right through her hand. Simple stuff for us. Easy to take care of. Three of us ran over. Two more than was necessary. An orthopedist playing ICU doc was walking by. He ran over. He was excited. We were all excited. This was not Covid. This was something we could fix. We did it together. Eight hands to do the job of two. We removed the needle, help it up like a trophy, washed it off and gave it back. Our patient smiled, said thank you, and went home in one piece. It was the best we’d felt in days.
//
My colleagues are tired. The patients keep coming. The ER is wall to wall misery and mayhem. Only five people died on me today. Only five. But everyone there is dying to varying degrees and at various rates. The ER is a cross section of the disease. The well who will stay well. The well who will come back much worse. The sick who are stable. The sick who are crashing. It’s all around us. It keeps coming in through the front door. It keeps coming in through the ambulance bay. And my colleagues are tired. We give oxygen. Everyone staying gets oxygen. Needs oxygen. We try antibiotics. We try antivirals. We try hydroxychloroquine. This week we use steroids. This week we limit IV fluids. This week we give blood thinners. Does anything work? Are we saving anyone or just supporting them as they go along a path pre-determined by the virus coursing through their insides? Is the inevitable inevitable? Some days we just feel like spectators, front row observers going through the necessary motions of a play whose final act has already been written. So much death. So much dying. And my colleagues are tired. We’re all tired. And yet somehow, for some reason, I find there’s no place I’d rather be. I leave the ER, the sun has come up and I walk around enjoying its warm tendrils. Its quiet. Stores are shuddered, streets are empty, and sidewalks are bare. It seems peaceful. Its an illusion. But I appreciate it. Time to go home. Time to recharge. Tired won’t last forever. Covid won’t last forever. And there is still plenty of fight in us.”
Imagine this being your current reality, then imagine what it must be like to see people protest the measures that are keeping that reality out of other communities. We’re not doing all of this for nothing. Yes, it’s frustrating, but we face nothing but frustrating options at the moment.
Thank you, Dr. Hill, for sharing your experiences and for doing your best to save lives. Let’s hope people see the warning in your words and act accordingly.