Ever seen how a sewing machine actually works? Even engineers' minds are blown by it.
"I'm a mechanical engineer and a grown man. I still consider a sewing machine to be a magical device."
Sewing machines are mechanical marvels.
Have you ever wondered how a sewing machine actually works? We've all likely seen some version of one, so we know you push a pedal, the needle goes up and down really fast, and fabric gets pushed through coming out the other side perfectly stitched.
But when you think about it from a hand-sewing perspective, it doesn't makes sense. With a sewing machine, the needle isn't being pulled all the way through the fabric—it's just the tip of the needle being inserted and pulled back out. Those of us who've used a sewing machine know there's bobbin thread that gets pulled from underneath to help form the stitch, but how? From the outside, it just looks like the needle and thread are going up and down, and yet the result is tight, perfect stitches of varying lengths and styles being created at incredible speed. How does it do it?
It turns out, it's not a dumb question. Veritasium created a video with a blown up model demonstrating how sewing machines work, and it's actually quite incredible. Despite being around for nearly 200 years, sewing machines are still a mechanical marvel, even to people who study engineering. As one commenter wrote, "I'm a mechanical engineer and a grown man. I still consider a sewing machine to be a magical device."
- YouTubeyoutu.be
As the video explains, sewing machines couldn't be made without first inventing a whole new way of sewing. Sewing machines aren't just a faster version of hand sewing—they create stitches in a whole different way that doesn't require a needle to go all the way through the fabric and then be reinserted.
For tens of thousands of years, humans have created sewing needles out of bone or wood that are all pretty much the same—sharp tip on one end, hole for thread on the other. But a sewing machine needle puts the hole at the same end as the sharp point. That gets the thread through the fabric without pulling the whole needle through. Then it's just a matter of catching the thread and tangling it to keep it from pulling out when the needle is pulled out.

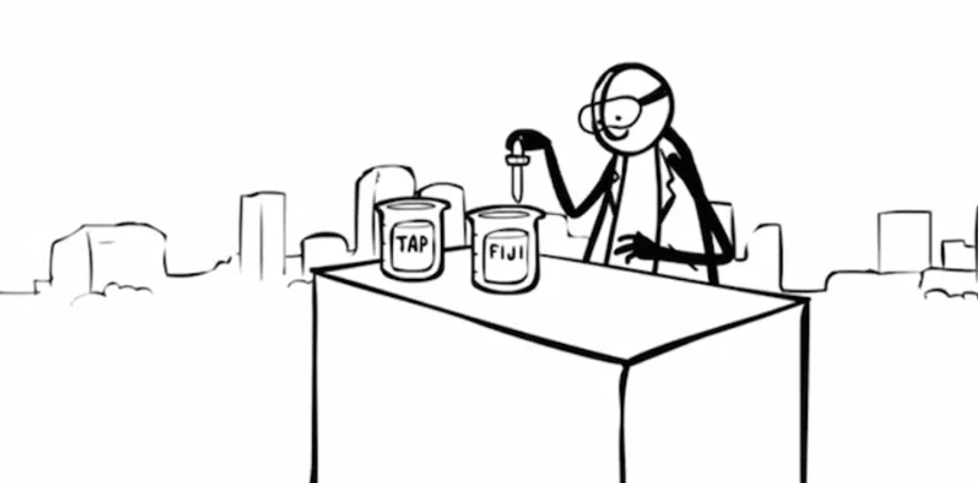
The story of the sewing machine is actually a story of many innovators coming up with ideas and then building on one another's models. Early sewing machine patents used a hook below the needle that either went back and forth or rotated to grab the thread and pull it forward as the needle went up, creating a simple chain stitch. The chain stitch works as long as no one pulls on the loose end, as the chain stitch is easily undone. (The demonstration in the video is really a must see for this.)
More complex chain stitches were created to solve this problem, but it was the lock stitch using two separate thread sources that really made the sewing machine the titan of inventions that it truly is. The bobbin thread gets intertwined with the needle thread, creating a stitch that can't be pulled out. There have been two main version of the lockstitch machine, one that used a shuttle that moved back and forth and one that most machines today use, which is the round bobbin hook.

The last sewing machine problem to solve was moving the fabric through the machine at an even pace. A grooved metal "foot" was attached that moved with the rhythm of the bobbin and needle to even move the fabric with each stitch. Simple, but genius.
Judging by the comments, many people had no idea how sewing machines worked before seeing this demonstration:
"At last! I have asked so many people how sewing machines work. I have looked at the machines, consulted experts, read manuals, and none told me how they work. I was amazed that people who worked with sewing machines for a living had no knowledge of, nor curiosity in, how they work."
"My mom, who is very good at sewing, didn't do it in a while because her machine wasn't set properly anymore after decades. As an engineer, I searched for the old instruction manual online, and carefully followed the instructions and oiled everything up : the machine was working flawlessly again. And I realized that I had NO IDEA of how it did work in the first place. So she explained it to me. I was literally amazed, so 1) seeing your video and your own amazement is so pleasing to me, and 2) blessed be my mom."

"I just got a vintage singer. I want to learn to make my own curtains, and clothes. I only have a straight stitch, but being a nerd your video helped me learn how to use the sewing machine. Knowing how it works, helps to know how to thread and set up the bobbin. I watched a few videos and couldn't understand it from the basic steps they were showing. I had to know how it works first. Excellent!"
"I’m a mechanical engineer and forever promised myself to someday take time to figure out how sewing machines work. You crossed this item off my list in just 15 minutes. I owe you the pizza of your choice. Thank you!"
"I use sewing machines pretty much every day at work and the funny thing to me is that most of us prefer older mechanical machines over modern digital ones. The action is just so much smoother, the sound is better, the power and durability is better. If you have a well maintained vintage machine, it'll probably outlive your grandchildren."
It's hard to overstate how the sewing machine changed life on Earth for humans. Not having to hand sew clothing, bedding, furniture coverings, etc. has saved us countless hours of work and enabled mass production of textiles. (Unfortunately, it has also enabled "fast fashion" to proliferate, but that's really a human problem, not a mechanical one.) Pretty incredible how the engineering of sewing machines still manages to amaze people, even after nearly two centuries.




 Kitten Aww GIF by MOODMAN
Kitten Aww GIF by MOODMAN James Roh
James Roh James Roh
James Roh The paint companies are dying to know the secret formula for the new color.
The paint companies are dying to know the secret formula for the new color. A close-up of the human eye.
A close-up of the human eye.  Traditional strawberry farming takes up a lot of land.
Traditional strawberry farming takes up a lot of land.