Sarah Palin blamed Obama for her son’s PTSD. This vet was not having it.
Sarah Palin went political with her son's PTSD.
Early in 2016, the Palin family rocketed back into headlines for a couple reasons.
On Jan. 19, 2016, Sarah Palin formally endorsed Donald Trump for president. Seeing as Trump's the current GOP front-runner and Palin was once gunning for the vice presidency, the endorsement naturally made waves.
Photo by Aaron P. Bernstein/Getty Images.
That same day, however, a different story cropped up regarding the Alaskan family. Track Palin, the former politician's 26-year-old son who served in Iraq, was arraigned on charges of domestic assault and possession of a firearm while intoxicated, USA Today reported. According to his mom, Track is living with PTSD (post-traumatic stress disorder), which played a role in her son's actions.
The two stories seemingly have nothing to do with one another. But Palin used the spotlight from her Trump endorsement to not-so-subtly blame her son's PTSD on Obama's failure to provide adequate resources to returning men and women in uniform. She stated that veterans "have to question if they're respected anymore" and they need a commander-in-chief "who will respect them and honor them."
If you're bothered by Palin's assertion that the president is somehow personally responsible for her son's wrongdoing, you're not alone.
On Jan. 20, Paul Rieckhoff, founder and CEO of Iraq and Afghanistan Veterans of America (IAVA), spoke out against Palin's dangerous message to voters, loud and clear.
"It's not President Obama's fault that Sarah Palin's son has PTSD," Rieckhoff, who served as an Army first lieutenant and infantry rifle platoon leader in Iraq, told NBC News. "PTSD is a very serious problem, a complicated mental health injury, and I would be extremely reluctant to blame any one person in particular."
Paul Rieckhoff speaks at an event in New York City. Photo by Jemal Countess/Getty Images.
Let's set aside the fact Obama has fought for veterans in a number of ways — like expanding their access to education, passing tax incentives encouraging businesses to hire them, and, yes, improving health care for those living with PTSD — it shouldn't even matter. Blaming a president for any one individual's battle with PTSD defies reason.
Rieckhoff — whose organization is bipartisan — called on Palin to "resist the urge to politicize" PTSD, and he encouraged Trump to provide specific plans on how he'd help vets living with the condition.
PTSD amongst vets is a serious issue that should be discussed by our leaders, but not in such a blatantly politicizing (and misleading) way.
PTSD surfaces when an individual's "fight-or-flight" response — a healthy, instinctive reaction every human has in times of distress to protect us from danger — is damaged or changed, according to the National Institute of Mental Health. The condition can arise after someone experiences something particularly terrifying — like abuse, rape, natural disaster, or war — and some research suggests it can even be inherited.
PTSD may cause a person to relive upsetting memories, experience jumpiness, and have trouble sleeping, among other symptoms.
A person living with PTSD may try to cope with their condition by abusing drugs and alcohol, according to the VA. Photo by Chris Hondros/Getty Images.
Because they are more likely to see violence abroad, war veterans are especially affected by PTSD. While about 7-8% of the general population will have the condition at some point in their lives, up to 20% of Iraq and Afghanistan war veterans will experience PTSD in a given year, according to the U.S. Department of Veterans Affairs.
"You may have been on missions that exposed you to horrible and life-threatening experiences," the VA's website says. "You may have been shot at, seen a buddy get shot, or seen death. These types of events can lead to PTSD."
Photo by Armend Nimani/AFP/Getty Images.
But it's not just related to combat trauma — female veterans are more likely to experience PTSD due to sexual violence experienced while serving too.
As Rieckhoff pointed out, the causes and ramifications of PTSD are complicated as they pertain to any one person. Palin's attempt to connect her son's mental health directly to a political foe is ignorant at best and malicious at worst.
Taking care of our vets should be a high priority for whoever lives in the White House in 2017 — Democrat or Republican.
One good thing that came from Palin's PTSD comments is that we're talking about the issue. Hopefully a candidate's platform in helping our returning vets will be a priority to voters this November.
Click here to support Iraq and Afghanistan Veterans of America.








 A woman reading a book.via
A woman reading a book.via A woman tending to her garden.via
A woman tending to her garden.via
 "The Magic Words" is a book of poetry prompts from Joseph Fasano.
"The Magic Words" is a book of poetry prompts from Joseph Fasano.  People with dementia are still themselves deep down.
People with dementia are still themselves deep down.  Caregivers try many different ways to communicate with people living with dementia.
Caregivers try many different ways to communicate with people living with dementia.
 Cats can be finicky about how they're held.
Cats can be finicky about how they're held.  Squish that cat.
Squish that cat. 
 Intelligent people are thoughtful.
Intelligent people are thoughtful. People who ask questions are often more intelligent.
People who ask questions are often more intelligent. People who can simplify big ideas concisely are more intelligent.
People who can simplify big ideas concisely are more intelligent.
 The doctors went in to remove Stuthers' tumor and go more than they bargained for. Photo by
The doctors went in to remove Stuthers' tumor and go more than they bargained for. Photo by 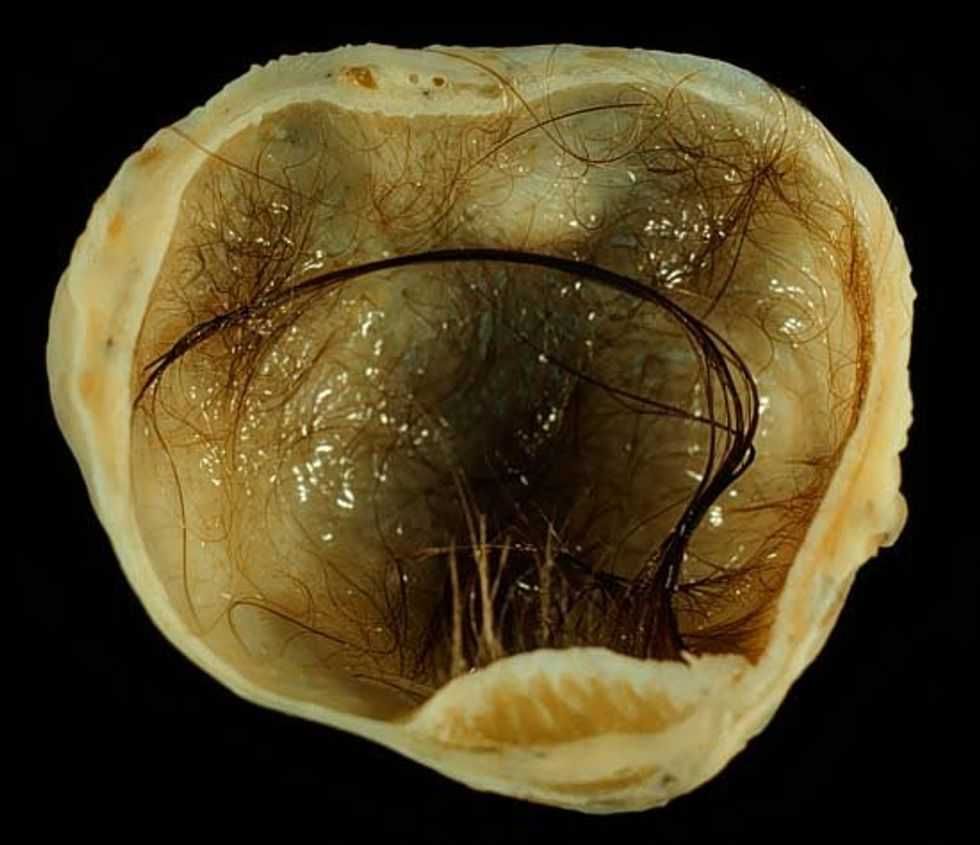 A teratoma with lots and lots of hair growth. Ed Uthman, MD. - Public Domain
A teratoma with lots and lots of hair growth. Ed Uthman, MD. - Public Domain  An ovarian teratoma with a long strand of visible hair. E.dronism/Wikimedia Commons
An ovarian teratoma with a long strand of visible hair. E.dronism/Wikimedia Commons