To be human is to navigate a complex world of pretense and subterfuge. You gotta fake it 'til you make it. You have to look the part and play the role. You tell white lies to help others save face and to adhere to rigid cultural norms that are too ingrained to bother challenging.
That's not to say it's all bad. Culture is always evolving, and some behaviors and attitudes that are completely "normal" in one period are seen as completely backward just a few years later. Just 40 years ago, corporal punishment of children was normal, mental health issues were seen as personal weakness, and sexual harassment in the workplace was rampant.
Things do get better, but first we have to point them out. Recently, a Redditor asked, "What's a social norm that you think is absolutely ridiculous?" to highlight today's cultural norms that people find absurd. Many commenters pointed out the excuses and white lies we tell in our social lives to avoid making our friends (and ourselves) uncomfortable. Others called out rigid gender roles we take for granted but deserve questioning.
Here are 15 social norms that people find "absolutely ridiculous"
1. The expectation that women have to wear makeup
"The expectation that women must wear makeup to look professional. A clean, washed face should be professional enough for any job i think."
"And being asked if you are sick or tired just because you aren't wearing a full face of makeup."
 A woman putting on makeup.via Canva/Photos
A woman putting on makeup.via Canva/Photos
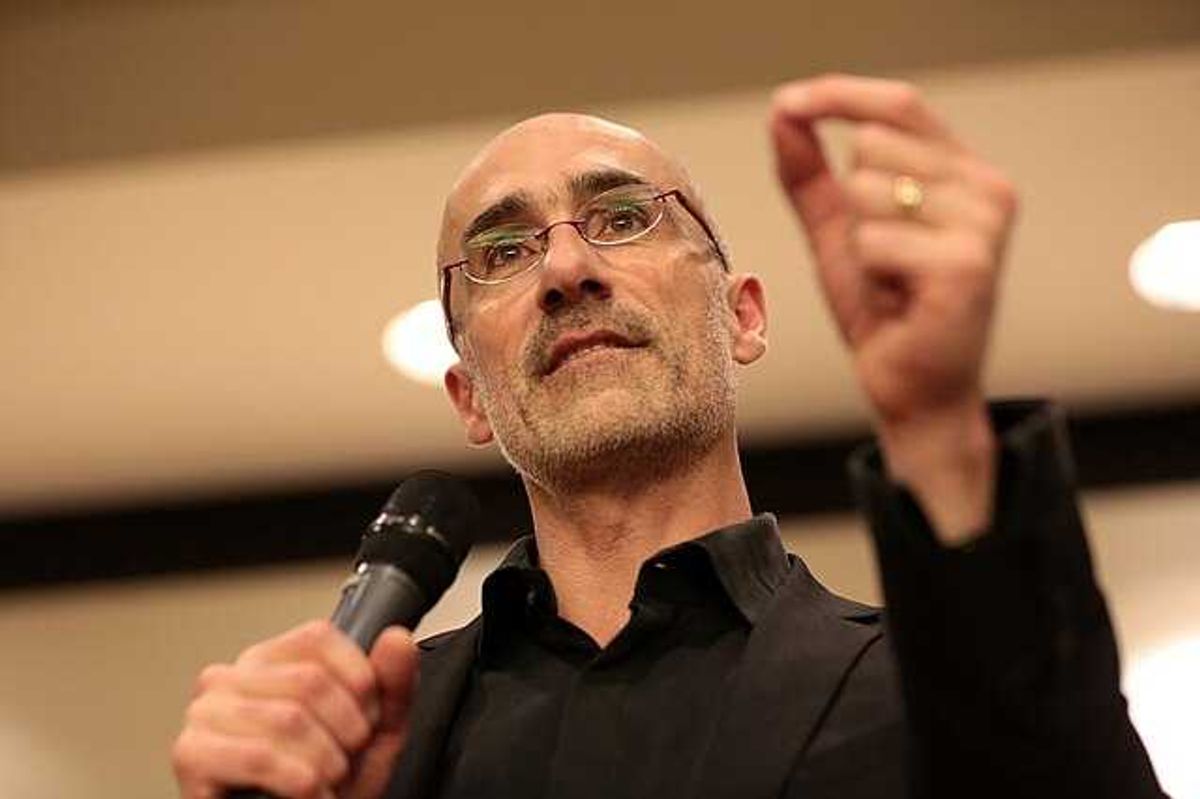
2. Faking workplace passion
"Pretending to be passionate about jobs in interviews when everyone knows it's just to pay bills."
"I applied to McDonald's in college and they asked me why I wanted the job. I said, very calmly, 'I need money and you need people, I don't understand the question.' Recruiter almost fell under the table laughing, I don't think he expected a blunt answer like that."
3. Having to justify turning down an invite
"People often feel they can't just decline an invitation or request with a simple I can't make it or 'that doesn't work for me instead there's this pressure to provide a detailed justification or excuse that proves you have a 'legitimate' reason. And if your reason is just 'I don't want to' or I need time to myself that's often not considered acceptable."
"'Don't make excuses. Your friends don't need them, and your enemies won't believe them,' — unknown."
4. Why we can't judge the dead
"Acting like someone was wonderful just because they're dead. There are absolutely some people that get and deserve a good riddance."
"It really rubs me the wrong way when a person who did or said terrible things died and suddenly all is forgot and they're a hero."
5. Influencers creating in public
"Turning public spaces into personal film studios for content creation and then getting mad when the public does public things and interrupts said content creation."
"This is not a norm. It's rude and should be treated as such. We were at the Louvre last year, and some influencer was trying to get people to move away from 'Liberty Leading the People' so she could film herself contemplating it. Lady, it's the size of a pickleball court. No one gets that much space to themselves there. She was so angry that other people kept looking at the art."
 An influencer filming himself.via Canva/Photos
An influencer filming himself.via Canva/Photos
6. Why we always have to be reachable
"Probably the whole 'always be reachable' thing. Like, if you don't reply to a message within 10 minutes, people assume something's wrong, or you're mad. Sometimes I'm just eating or staring at a wall, man. I think phones have blurred the line between urgent and not urgent, and now everyone feels low-key on call all the time. Would be nice if slower replies were normal again."
7. Oversharing on social media
"Everyone posting every aspect of their lives on social media for all to see."
"We should all know less about each other."
Why do some people overshare? In a 2022 study, researchers identified three main reasons. First, people tend to overvalue the positives and undervalue the risks when posting online. They overestimate the benefits and underestimate the downsides of oversharing. Second, oversharing has been linked to anxiety, with some people posting as a way to cope with difficult feelings. Finally, because people often feel relatively anonymous online, even when their name and face are attached to a post, they may feel freer to overshare.
 A woman taking a photo of herself in her bedroom. via Canva/Photos
A woman taking a photo of herself in her bedroom. via Canva/Photos
8. Elbows on the table being considered rude
"That was a social rule from the medieval age - tavern 'tables' were planks of wood laid on top of stumps. If someone put their elbows on that plank, the whole table would see-saw and chuck everyone's refreshments across the room."
"I was taught that it's because it seems like you're guarding your food, like an animal."
It's believed that the "elbows on the table" rule dates back to the Middle Ages, when feasts and festivals were jam-packed affairs and people were crammed around tables. Placing your elbows on the table, like spreading your legs on the subway, meant your neighbor had less room. You might even knock an elbow into their blackbird pie.
9. The need to be intoxicated
"The need to have alcohol at social events otherwise they are not fun or worth it to go to. Peer pressuring folks for not wanting to drink and making them out to seem boring or unfun. Having drug usage/alcohol as a personality trait."
"I tell people I'm straight edge, and they look at me like I'm some kind of monster. I once got told, to my face, someone who has never drank or smoked or done a drug is not a trustworthy person."
 A drunk guy passed out.via Canva/Photos
A drunk guy passed out.via Canva/Photos
10. Period shame
"Acting like periods are something to be ashamed of. Never understood as a teenager why people would smuggle their pads into the toilet or whisper about their period or peel back the wrappers really quietly so no one else could hear it. It's completely natural and nothing to be ashamed of. I make an effort as an adult to openly carry pads and talk about it openly. We need to stop acting like it's a big taboo!"
11. Taking the man's last name
"Women and children taking the man's last name by default."
"I think you should have to smoosh the names together to make a new surname, and if you get remarried, you keep smooshing names."
12. Men have to propose
"Believing the male partner in a straight relationship must be the one to propose marriage."
"Or believing that a proposal has to be a grand gesture. My husband proposed to me on his front porch with, 'Hey, you don't happen to want to marry me or anything, do you?' Was it romantic? No. But he did manage to get the point across. This summer we'll be married 38 years."
13. Wearing a tie
“'Humans are the only species that start the day with a noose around their necks,' Source : unknown."
"I still wish we adopted the double necktie as seen in Back to the Future Part II in the far distant future of 2015."
 A man adjusting his tie.via Canva/Photos
A man adjusting his tie.via Canva/Photos
14. Smartphones being everywhere
"I've seeing a lot of waiting rooms lately, and I'm trying to just sit there without looking at my phone, and I'm realizing how captivating it is. Everyone is plugged in."
"I agree it's great. As an introvert, to look up and realise NO ONE IS LOOKING AT YOU is like being king of that little space."
15. Saying you're "fine" when you're not
"Being expected to say 'fine' when someone asks how you are, no matter how not fine you feel. Also apologizing when someone else bumps into you, and pretending emails need fake pleasantries instead of just getting to the point."
"Some days when life isn't fine, and someone asks me how life's going, I tell them it's certainly going, they should get the message at that point."









 A woman is getting angry at her coworker.via
A woman is getting angry at her coworker.via  A man with tape over his mouth.via
A man with tape over his mouth.via  A husband is angry with his wife. via
A husband is angry with his wife. via 
 Many people make bucket lists of things they want in life.
Many people make bucket lists of things they want in life. 

 A woman putting on makeup.via
A woman putting on makeup.via  An influencer filming himself.via
An influencer filming himself.via  A woman taking a photo of herself in her bedroom. via
A woman taking a photo of herself in her bedroom. via  A drunk guy passed out.via
A drunk guy passed out.via  A man adjusting his tie.via
A man adjusting his tie.via