There's a lot of talk around bad or unconvincing accents in Hollywood movies. Lines, scenes, or entire films that just don't quite sound right. But there are just as many, or more, examples that are absolutely brilliant.
One of my favorite recent examples is Tom Holland in the Spiderman films. Holland is British, and sounds like it in real life. Yet in the Marvel movies, he perfectly passes for a young American kid speaking plain old English. I can't imagine how much work it must take for him to (seemingly effortlessly) sound like an American! Andrew Garfield (ironically, another Spiderman) also does a commendable American accent, as does Idris Elba. Meryl Streep is world-renowned for her accent work in movies. Cate Blanchett is another actress that's consistently lauded for accurate dialects. The list goes on and on.
Have you ever wondered how certain actors get so good at accents? Of course, they have coaches to help them but do some people just have a natural ear for replicating dialects?
Well, yes, some people do have a natural ear and talent for accents. But there's an incredible phonetic tool that some actors use to master their accent work. It's a special alphabet that anyone can learn, and it can enhance your ability to speak any language fluently and convincingly.
And most people have never heard of it!
Learning any language, even your own native language, requires a fair bit of memorization. Pronunciation cues aren't always obvious in the written language. Duolingo astutely points out that the u in 'dude,' 'put,' and 'putt' makes a slightly different sound in each word.
We know the e at the end of 'dude' makes the long u sound. But what explains the difference between putting (like golf) or putting (as in, to put) and the difference between pudding and puddle?
Unless you've memorized the near-entirety of the English language (the way we do slowly as we grow up surrounded by it), you'd have a nightmare of a time trying to pronounce it all properly. Add in tongues, accents, and dialects that alter the rules as we know them of language, and you can imagine how difficult it would be for, say, a person who grew up speaking Spanish trying to learn a specific flavor of New York English.
This is where the International Phonetic Alphabet (IPA) comes in. It's a universal organizational system that categorizes all the different possible vowel and consonant sounds the human mouth can make, and writes letters and words according to those sounds—not any one specific language's writing system.
So, when it comes to that pesky letter u, when using the IPA you won't have to guess what sound it makes based on the letters that surround it.
The three U sounds would all be written differently: /u/, /ʊ/, or /ʌ/.
Conversely, there are several combinations of vowels in English that all make the same sound. 'Bead,' 'tree,' 'key,' and 'chic' all have the same vowel sound in the middle despite different spellings. Confusing! With the IPA, however, that sound would be written as /i/ regardless of what letters make up the sound. It's all about the mouth!
@vox.to.verbaReply to @thechronictrekkie #ipa #internationalphoneticalphabet #linguistics #linguistic #appliedlinguistics #ipachart #phoneticalphabet #phonetics #phoneticsandphonology
The phonetic alphabet is incredibly detailed in its cataloguing of sounds. There are terms and annotations that refer to the shape and position of your mouth and tongue as you create the sound, words that describe how much air you're letting out, whether your tone is rising or falling. It's absolutely incredible.
For example, the voiced alveolar tap is something of an "r" sound that involves tapping the tongue on the roof of the mouth. That's not to be confused with the voiced alveolar flap which has the tongue slightly curled before tapping. Fascinating!
Imagine being an actor trying to learn an Irish accent for a role. You can listen, and be coached, by a native speaker. But it might also be extremely helpful to break your lines down into the specific sounds and mouth shapes you'll need to master in order to sound truly authentic.
 Not exactly a light read, but if you're serious about mastering your pronunciation the IPA can be a huge help.International Phonetic Association, CC BY-SA 3.0
Not exactly a light read, but if you're serious about mastering your pronunciation the IPA can be a huge help.International Phonetic Association, CC BY-SA 3.0
You don't have to be an actor trying master an accent to learn the IPA and make good use of it.
Studying the IPA for a language you're trying to learn can rapidly accelerate your pronunciation. Phonetic spellings not only tell you the shape and movement of your mouth, it can also tell you which syllable in the word should get the emphasis and how your vocal tone should change throughout the word. That kind of learning can take you from someone who can merely stumble through a few sentences in a chosen language, to someone who can truly converse in it.
The phonetic alphabet is also heavily used in speech therapy. Therapists will create a phonetic transcription of a sample of speech in order to determine the nature of any errors or difficulties. That allows them to create a targeted treatment plan to address those specific errors.
@englishnativetongueNow I know my IPA I hope you learned with me today! 🎶 The English International Phonetic Alphabet (IPA) Song I saw @CoffeeCupEnglish do this song and I just had to try my best and recreate it with an American accent! #englishlanguage #englishlearning #ipasong #nativetongue
English is such a funny and tricky language. For every rule (of which there are many), there are twice as many exceptions. It's a wonder anyone can ever learn it.
And yet, English is the third most spoke language in the world, and one of the most universal. It's an extremely common second language for people in all corners of the globe, which sure is convenient for those of us born in America.
Somehow, I never knew there was an easier way to learn how to pronounce things. A way to bypass all of English's nonsensical rules and unspoken peccadilloes. If only the International Phonetic Alphabet wasn't such an eyesore on paper, maybe we could ditch the written version of English entirely. Then, of course, I would be out of a job!





 Some at-home perk simply can't be beat.
Some at-home perk simply can't be beat.  Mark (Adam Scott) at the infamous dance party scene in Severance.
Mark (Adam Scott) at the infamous dance party scene in Severance.  A
A  A man and woman chatting.via
A man and woman chatting.via  Coworkers having a conversation.via
Coworkers having a conversation.via  Coworkers having a conversation.via
Coworkers having a conversation.via  Rachel Ruff Cuyler explaining how she would "fix" Poolhouse' song to make it the next "Teenage Dirtbag." @rachelruffcuyler/
Rachel Ruff Cuyler explaining how she would "fix" Poolhouse' song to make it the next "Teenage Dirtbag." @rachelruffcuyler/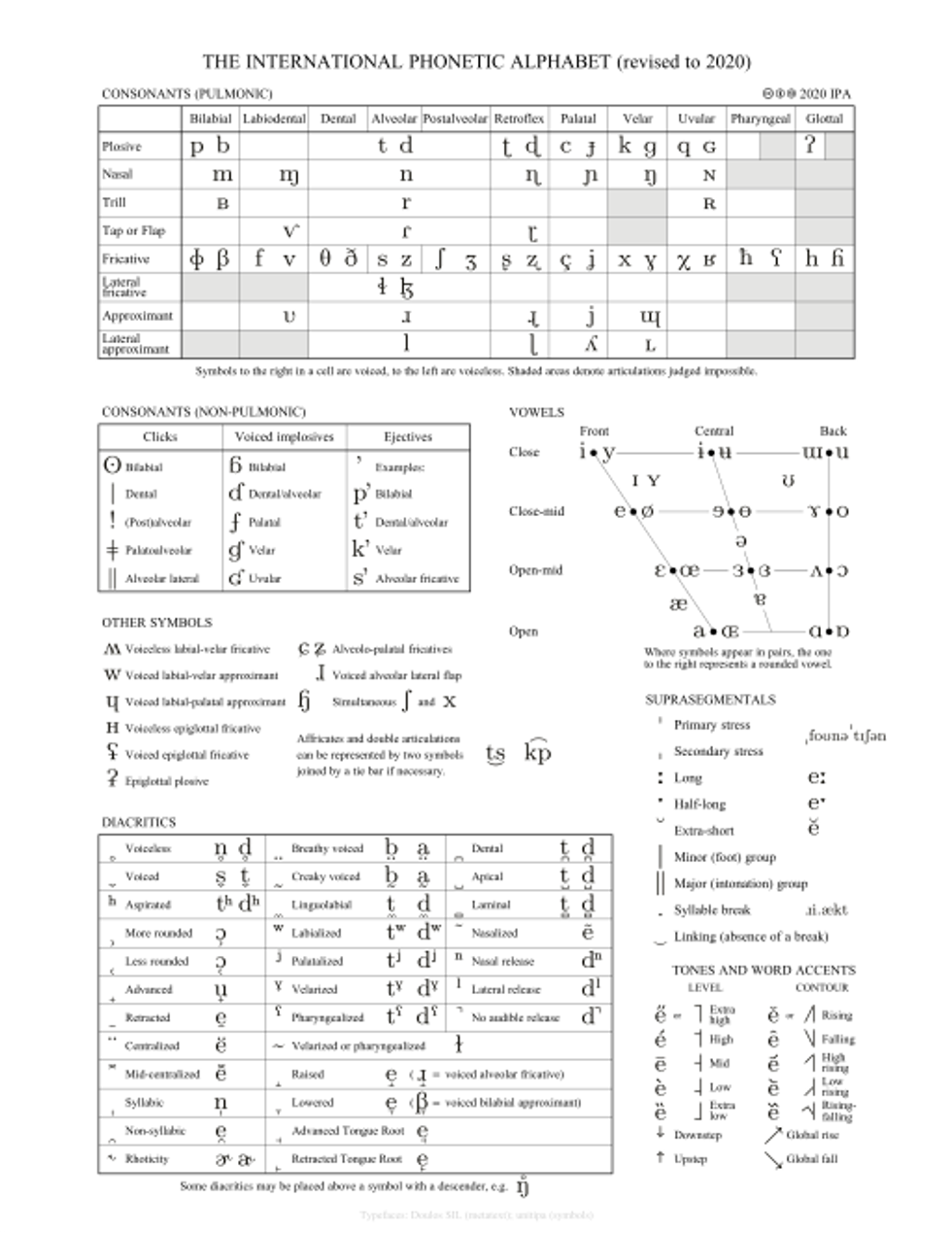 Not exactly a light read, but if you're serious about mastering your pronunciation the IPA can be a huge help.International Phonetic Association, CC BY-SA 3.0
Not exactly a light read, but if you're serious about mastering your pronunciation the IPA can be a huge help.International Phonetic Association, CC BY-SA 3.0