A man died suddenly during a brain scan. What scientists saw was beautifully comforting.
Death may not be scary or painful after all.
A man had a heart attack and died while having his brain waves measured. The data was eye-opening.
Death remains a very difficult topic for scientists to study. While there are some reports of near death experiences (NDEs) or people being revived after being declared dead, we've never been able to definitively confirm what happens beyond the grave. Further complicating things, death is often either sudden and unexpected, or a slow and drawn-out process. It's hard to get accurate readings and measurements at the exact moment someone passes away.
However, in 2021, researcher Dr. Raul Vicente and his colleagues at the University of Tartu, Estonia, became the first people ever to record the brainwaves of someone in the process of dying, and what they’ve come to realize should be very comforting to everyone.
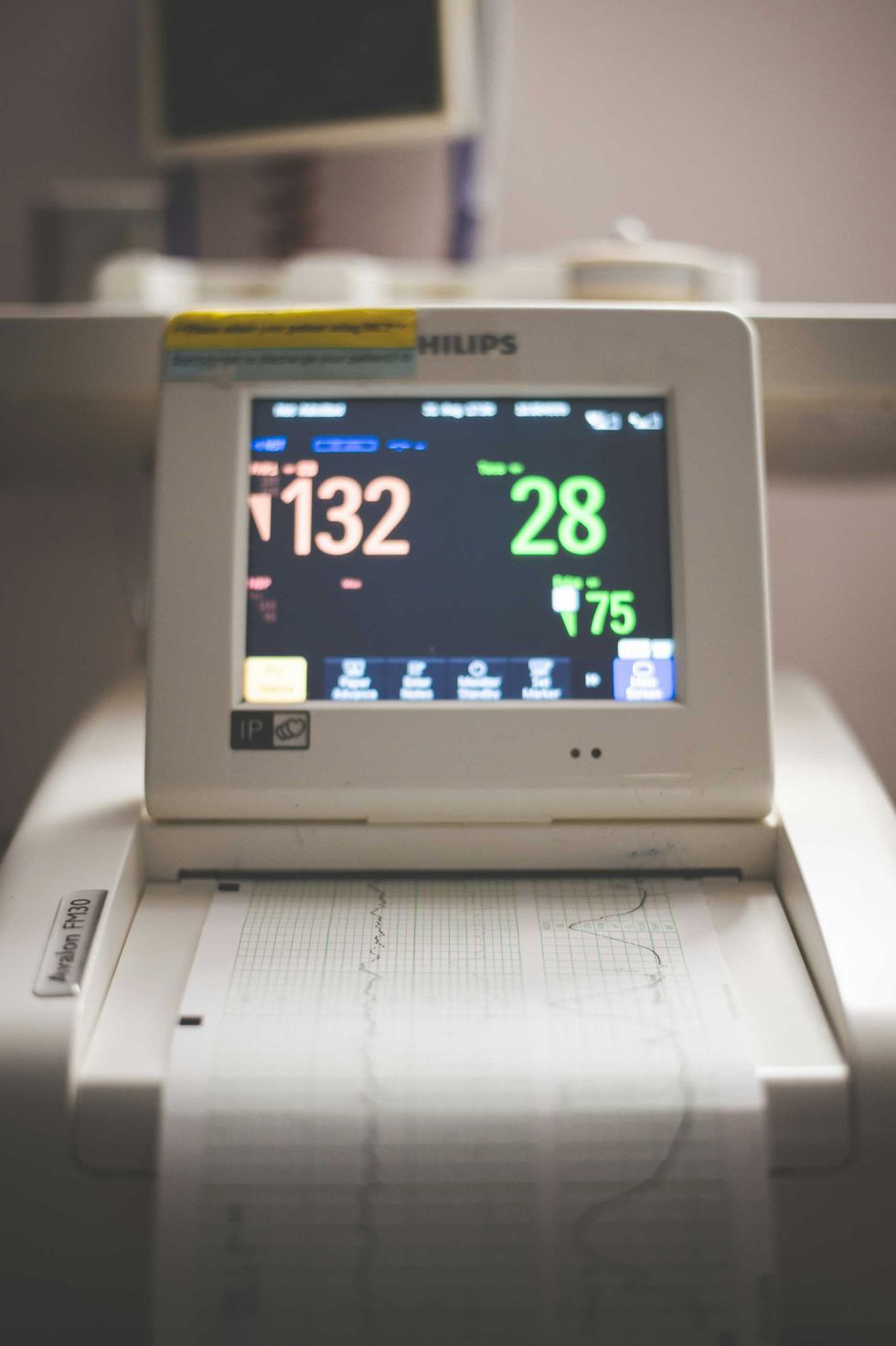
“We measured 900 seconds of brain activity around the time of death and set a specific focus to investigate what happened in the 30 seconds before and after the heart stopped beating,” Dr. Ajmal Zemmar, a neurosurgeon at the University of Louisville, US, who organized the study, told Frontiers.

Fascinatingly, the discovery was a complete accident.
The patient who died while having his brain waves measured was 87 years old and had epilepsy. While researchers were studying his brain to learn more about the condition, the man had a heart attack and passed away. “Just before and after the heart stopped working, we saw changes in a specific band of neural oscillations, so-called gamma oscillations, but also in others such as delta, theta, alpha, and beta oscillations,” Zemmar said.
The findings were so special and rare because the man just happened to be hooked up to machines that could measure his brain waves; a miraculous coincidence.
- YouTube www.youtube.com
The different types of brain oscillations that occurred in the patient before and after the heart attack were associated with high cognitive functions, including dreaming, concentrating, memory retrieval, and memory flashbacks.
Therefore, it’s possible that as the patient was dying, they had their life flash before their eyes. What an amazing and comforting experience right before leaving this mortal coil.
“Through generating oscillations involved in memory retrieval, the brain may be playing a last recall of important life events just before we die, similar to the ones reported in near-death experiences,” Zemmar speculated. “These findings challenge our understanding of when exactly life ends and generate important subsequent questions, such as those related to the timing of organ donation.”
The positive findings line up with reports of NDEs and first-hand observations from hospice workers. Medical workers who work with dying folks report they often have visions of visitations and conversations with deceased loved ones, almost as if those relatives and friends are preparing to guide them over to the other side. Many people who have been declared dead and lived to tell the tale, or suffered an extreme NDE, report feelings of calm and peace rather than fear and pain.
How long are people conscious after they are technically dead?
Science has found that people can remain conscious up to 20 seconds after they are declared dead. Even after the heart and breathing have stopped, the cerebral cortex can hang on for a little while without oxygen. So, some people may experience the moment when they hear themselves declared dead, but they aren’t able to move or react to the news. In cases where someone performs CPR on the deceased person, the blood pumped by the compressions can temporarily keep the brain alive as well.
Although the experience of death will probably always remain a mystery, we should take solace in the idea that, in many cases, it may not necessarily be a miserable experience but an ecstatic final burst of consciousness that welcomes us into the great beyond. “Something we may learn from this research is: although our loved ones have their eyes closed and are ready to leave us to rest, their brains may be replaying some of the nicest moments they experienced in their lives,” Zemmar concludes.
This article originally appeared in February. It has been updated.
- Thousands of people explained why they're not afraid of dying. Here are their top reasons. ›
- Hospice nurse shares clue she uses to know if someone is dying 6 months before it happens ›
- A dying woman left a heartwarming note to her cat’s future owner. ›
- Poet Andrea Gibson reads 'Love Letter From the Afterlife' to fiancée just months before dying ›

