Eight months into the coronavirus pandemic and it feels like disinformation and denial have spread as quickly as the virus itself. Unfortunately, disinformation and denial during a pandemic is deadly. Literally. People who refuse to accept the reality we’re living in, who go about daily life as if nothing unusual were happening, who won’t wear a mask or keep their distance from people, are preventing communities from being able to keep the pandemic under control—with very real consequences.
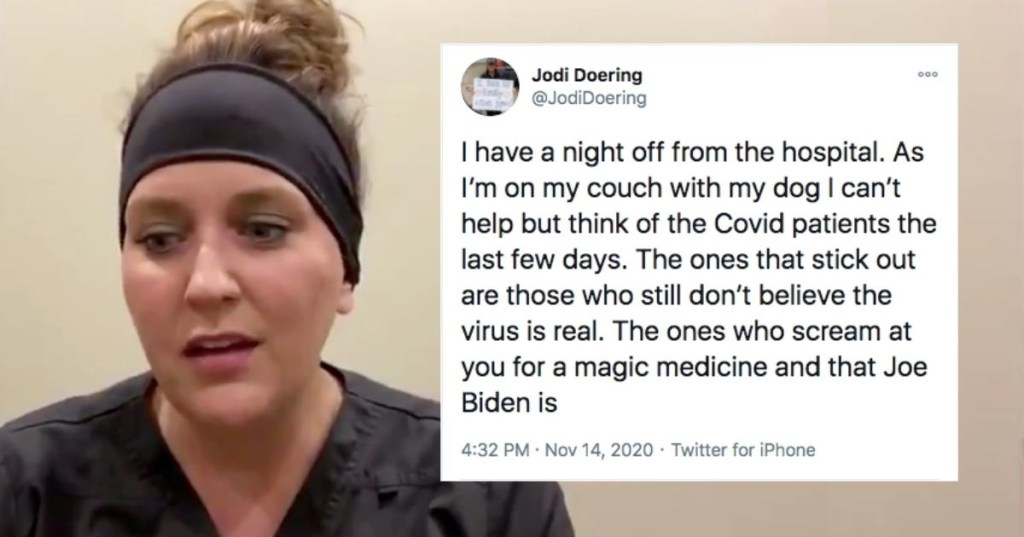
An ER nurse in South Dakota shared her experience treating COVID patients—some of whom refuse to believe they have COVID—and it’s really shocking. One might think that the virus would become real to people if they were directly affected by it, but apparently that’s just not true for some. As Jodi Doering wrote on Twitter:
“I have a night off from the hospital. As I’m on my couch with my dog I can’t help but think of the Covid patients the last few days. The ones that stick out are those who still don’t believe the virus is real. The ones who scream at you for a magic medicine and that Joe Biden is going to ruin the USA. All while gasping for breath on 100% Vapotherm. They tell you there must be another reason they are sick. They call you names and ask why you have to wear all that ‘stuff’ because they don’t have COViD because it’s not real. Yes. This really happens. And I can’t stop thinking about it. These people really think this isn’t going to happen to them. And then they stop yelling at you when they get intubated. It’s like a fucking horror movie that never ends. There’s no credits that roll. You just go back and do it all over again.”
Doering’s Twitter post went viral, and CNN’s New Day invited her to come on the show. Her interview is stunning and sad, as she explains how patients who should be spending their final hours talking with their loved ones spend them ranting about how the virus is all a hoax.
“I think the hardest thing to watch,” she said, “is that people are still looking for something else and they want a magic answer and they don’t want to believe COVID is real. And the reason I tweeted what I did was it wasn’t one particular patient, it’s just a culmination of so many people. And their last dying words are ‘This can’t be happening. It’s not real.” And when they should be spending time Facetiming their families, they’re filled with anger and hatred, and it just made me really sad the other night. I just can’t believe that those are going to be their last thoughts and words.”
Doering explained that nurses can handle people lashing out at them in anger (bless you, nurses) but when they ask patients if they want to Facetime their families when they are clearly not likely to recover and they refuse, it’s just sad.
“I think people look for anything,” she said, when asked what people think is wrong with them if they don’t believe it’s COVID. “People want it to be influenza, they want it to be pneumonia…we’ve even had people say ‘Well I think it might be lung cancer.’ I mean, something so far fetched, and the reality is, since day one when COVID started in this area in March, you’ve kind of been able to say if it walks like a duck and talks like a duck, it’s a duck…even after positive results come back, some people don’t believe it.”
Doering made it clear that not all patients are living—and dying—in such denial. But the deniers are memorable. “It’s just a movie where the credits never roll,” she said. “You just do it all over again. And it’s hard and sad because every hospital, every nurse, every doctor in this state is seeing the same things. These people get sick in the same way, you treat them the same way, they die in the same way, and then you do it over again.”
The medical community has learned a lot about how to treat the virus, and Doering says they are managing their patient load fairly well. But the numbers keep climbing. South Dakota has a 50% positivity rate, which is astronomical. (The CDC guidance on school reopenings recommended that schools should only consider opening when positivity rates are below 3%, for a frame of reference.)
The virus is real, the pandemic is real, the illnesses and hospitalizations are real, and the deaths are real. We’ve got to figure out a way to pull deniers back to reality for everyone’s sake, including their own.