Ask any social scientist and they’ll agree: Humans are really, really, really good at having sex.
But, for as long as we’ve been having it, we’ve also been trying to prevent some of the less desirable things that sometimes come along with it — namely unwanted pregnancies and STIs.
Modern science and medical innovation give sexually-active people lots of safe and reliable options to do both, and condoms, in particular, are now extremely effective — preventing pregnancy and STIs about 98% of the time when they’re used correctly.
Getting to this point wasn’t a quick process though. It involved centuries of trial and error, some terrible ideas (two words: dung sponges), and some serious medical breakthroughs.
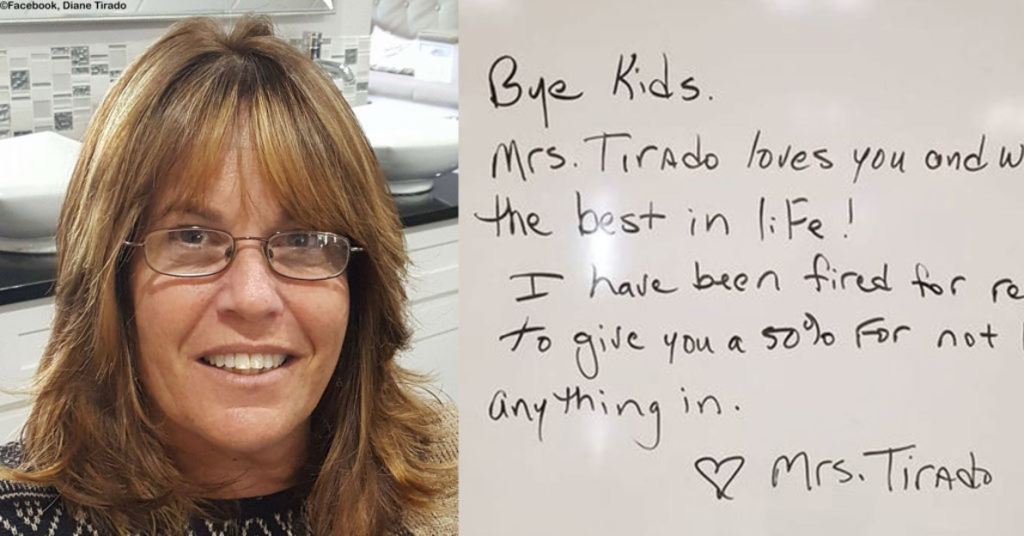
A condom from 1813 that might be a bit beyond its expiration date. Image via Lund University Historical Museum/Wikimedia Commons.
Condoms can be traced back to about 3,000 B.C.
According to Greek mythology, King Minos of Crete and his wife, Pasiphaë, used a goat’s bladder as a barrier during sex, after several of Minos’ mistresses died from the “scorpions and serpents” in his semen.
Over the next several thousand years, Greek, Roman, New Guinea, Chinese, and Japanese civilizations developed and used their own condom variations for women and men using linen, animal bladders, intestines, or a combination of the three. While evidence of condom use continued to appear in art and literature for hundreds of years, it took until the 16th century for a doctor to apply scientific methods to test their effectiveness.
That doctor was Gabriel Fallopius, and his work greatly advanced the human understanding of reproductive health.
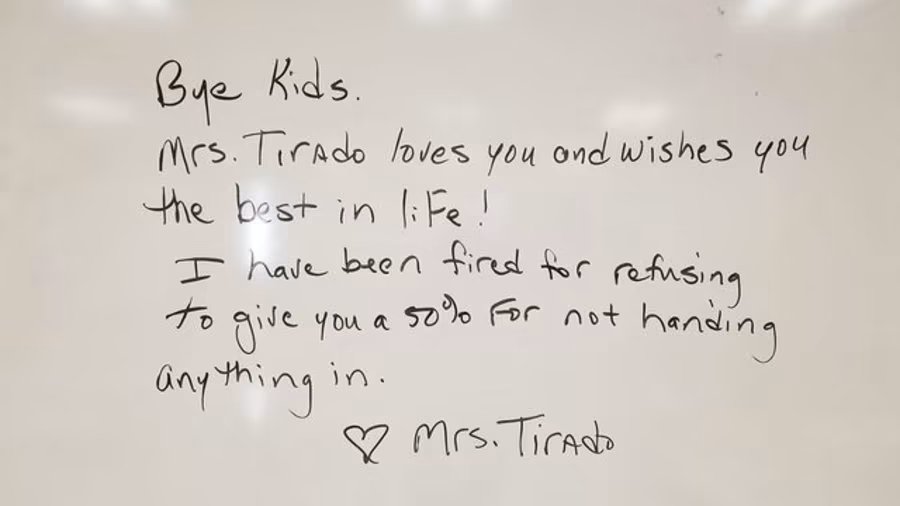
An etching of Gabriel Fallopius. Lin-Manuel Miranda hasn’t written a musical about his mostly-unknown legacy yet, but he absolutely could. Image via Wellcome Images/Wikimedia Commons.
By his early-thirties, Fallopius was already considered one of the greatest anatomical researchers of the time. He studied the muscles of the head, the workings of the inner ear, and the nerves and muscles of the human eye. He disproved the theory that the penis entered the uterus during sex. He proved the existence of the hymen in women and discovered the tubes (now called fallopian tubes) connecting the uterus to the ovaries. He reportedly coined the word “vagina” and was the first to describe the clitoris.
With an extensive knowledge of reproduction and biology, Fallopius turned his attention toward the prevention of STIs — namely, syphilis.
“A Harlot’s Progress,” a famous 17th century etching by William Hogarth featuring a fictional British prostitute, Moll Hackabout, dying of syphilis. Image via The British Museum/Wikimedia Commons.
By the 16th century, syphilis infections had reached epidemic levels across western Europe. Early stage sufferers would endure rashes, joint pains, and fever. Late stage sufferers could go blind, experience heart problems, mental disorders, nerve problems, and eventually, die. Even worse, men and women were carrying the disease unknowingly, contracting it and then passing it on again without ever showing symptoms until they were past the point of treatment. Women of childbearing age were at an added risk because they could pass their infection on to their unborn children, causing birth defects, such as deformed noses, misshapen teeth, blindness, and deafness.
Fallopius and his contemporaries knew enough about syphilis to know that it was transmitted through sexual contact. He further deduced that a barrier preventing the genitals from touching directly during sex could reduce the risk of exposure.
The solution? A thin linen sheath soaked in herbs and unnamed chemicals and then dried.
Men, Fallopius surmised, could wear the sheath during sex — reportedly tied with a ribbon — and potentially prevent infection.
It was a fascinating and simple idea. The next step was proving it worked.
In what is considered to be one of the first historical examples of a clinical trial, Fallopius recruited 1,100 men to test out a sheath during sex.
Gabriel Fallopius describes some of his discoveries to the Cardinal Duke of Ferrara. Painting by Francis James Barraud. Image via Wellcome Images/Wikimedia Commons.
The results were astonishing: not one single participant reported contracting syphilis while using the sheath.
In a book about the experiment published two years after his death, Fallopius reported on his findings: “I tried the experiment [the use of condoms] on 1,100 men, and I call immortal God to witness that not one of them was infected.”
Unlike a modern clinical trial, which would confirm patient reports with tests, Fallopius had to trust his participants to tell the truth. Still, the trial was a major breakthrough in STI prevention — and in our collective understanding of the transmission of this deadly disease.
Centuries later, the condom continues to evolve.
Simple, portable, and life-saving. Image via iStock.
Linen and animal intestine sheaths have been replaced with latex, polyurethane or polyisoprene. There are female condoms and condoms of all sizes and shapes for men. They are designed to improve pleasure for both partners, made increasingly thin with ridges, ripples, and other pleasurable accoutrements. Best of all, they’re inexpensive, readily available, and easily transportable.
Philanthropist Bill Gates is so convinced of the importance of condom use in aiding sexual wellness in developing countries that, in 2013, he awarded grants to designers who could make an effective condom that doesn’t limit sexual enjoyment. The winning design, an ultra-sensitive sheath made partly from bovine collagen, is awaiting approval from the FDA.
Condoms are far from perfect, but when used correctly by consenting partners, they give people more autonomy and control over their bodies.
And while there have been many innovations beyond what he ever dreamed of, we can collectively thank Gabriel Fallopius for his work in helping the science along to where it is today.