When I was 22, I decided to stop drinking.
Considering my history, the decision happened after a rather insignificant night.
It did not happen the morning I woke up in the hospital with hypothermia and alcohol poisoning.
It did not happen when I spent 30 days in rehab after getting into a drunken fight with my parents and chugging a bottle of mouthwash and a handful of prescription pills.
It did not happen after a 50-something bartender told me I needed to kiss him to get my ID back, which somehow led to me bringing him back to my dorm.
It did not happen after I had to run away from a homeless man who led me to a park and exposed himself to me after I asked for directions.
It did not even happen after I almost left a New Delhi Men’s Fashion week party with a man who said he was a model but was actually a pimp and later tried to sell me an hour in a limo with a boy or girl for $400.
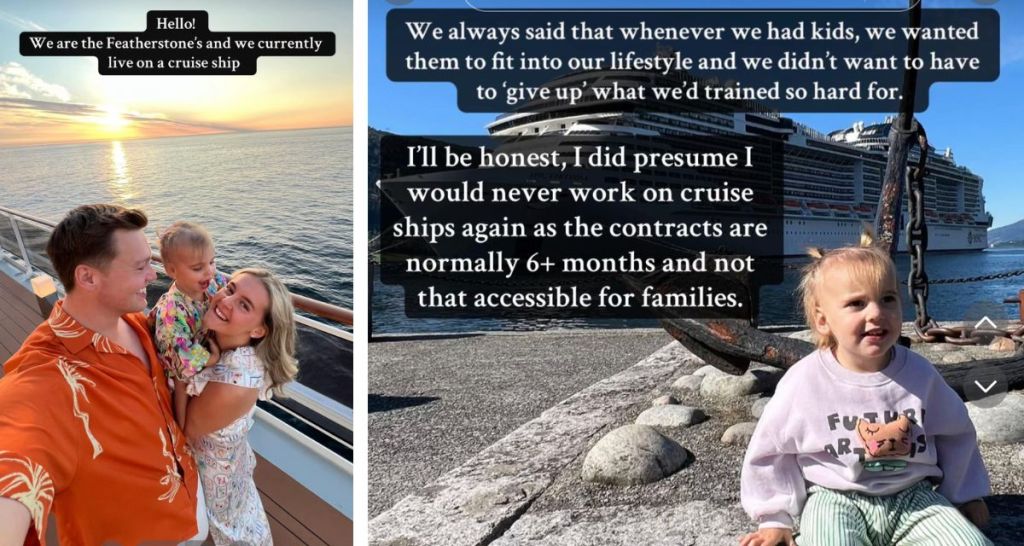
All photos provided by the author.
Instead, it happened after I had gone out drinking with my friends, blacked out, and had to be brought home. When I woke up in the morning, I felt like I was reaching the surface just as I was about to use my last breath of oxygen underwater. I had been so consumed by self-created chaos that I had not had clarity of mind for years.
“What if my friends hadn’t been there?” I asked myself. “What if they hadn’t brought me home?”
Of course, I already knew the answer. But for the first time, I allowed myself to let it sink in: If I didn’t stop drinking I was going to wind up killing myself, either intentionally or accidentally. And it was going to happen soon.
I had been drinking regularly since I was 15.
My issue with high school and college drinking was the blurry line between typical — if dangerous — experimentation and blatant drinking problems. It wasn’t bizarre that I hid a bottle of vodka beneath the floorboards in my parent’s attic, but I crossed beyond standard teenage rebellion when I poured vodka into my mug full of Sprite while doing homework.
As a gay teenager in an inner city high school, alcohol took on extra significance for me. Drinking is an equalizer: Anyone can do it. Though I loved my close friends, I always felt different, apart. I used alcohol as a means of bonding with classmates I otherwise had nothing in common with.
In retrospect, the truth was glaring and obvious, even then. By the time I graduated from high school as my class’s valedictorian, I had been hospitalized three times for alcohol poisoning, had completed a month-long stint in rehab, and had spent a night in a psychiatric center after a drug-induced breakdown.
I left for college with high hopes, but things only got worse.
I wanted to study international relations and become a human rights lawyer. But without the structure of high school, I quickly fell apart. I drank almost every night.
Where I had been admired for my work ethic in high school, in college, I schemed to do the bare minimum. I ignored the changes happening to me. I no longer took any joy out of learning or any joy out of much of anything at all besides partying.
I hid my past from my friends at Brown too, but as time went on, my troubling relationship with substances came to the surface again and again. By the time I graduated, I had been hospitalized again, I suffered from a Xanax addiction, and I had trouble sleeping at all. I was aggressive and reckless.
After college, I moved to New York without a job.
My lowest point came soon after when I drunkenly broke up with an ex-boyfriend at a party and tried to run into heavy New York traffic while two friends walked me home. They pulled me back. I was in a complete blackout. They told me I sobbed for an hour, then passed out.
That month, I convinced myself — and my therapist — that I would give drinking one last chance. We put rules in place limiting my alcohol consumption to three drinks on weekend nights. But over the next two weeks, I broke all the rules again.
The day I finally broke down was a Sunday, two weeks after the meeting with my therapist. I woke up in tears. I couldn’t remember the last time I’d felt well, and I was exhausted by the cycle of destruction and damage control I was putting myself through. In that moment, I knew the only way I might ever be happy was if I never drank again.
I couldn’t remember the last time I’d felt well, and I was exhausted by the cycle of destruction and damage control I was putting myself through.
On that New York morning two-and-a-half years ago, I finally allowed myself to be honest.
The thought of living the rest of my life in this state of dull despair finally felt much more impossible than saying goodbye to drinking.
If you’re a heavy drinker, the decision to stop drinking can seem impossible.
I’d always run with a hard-partying crowd. Plus, the thought of losing access to social situations can be terrifying. Whenever I would try to sober up — which happened at least 10 times before it actually worked — a voice inside my head would incessantly shout: “What if I’m less funny when I’m sober? What am I even going to talk to this person about if I’m not drunk? I can’t dance until I’ve taken a few shots! Sleeping with someone without alcohol?!”
Alcohol felt like my lifeline, and it was only on rare occasions — during common morning panic attacks — that I even briefly acknowledged it was actually destroying my life.
I can recognize now that deflection was my weapon of choice as an alcoholic. If I woke up frightened after a night of drinking, I would tell the story for a laugh. Though people would occasionally confront me, most acted as if I was entertaining. Besides, I quickly realized if my “partying” pushed a friend away, there were always five more people who wouldn’t notice, or care, how many drinks I had or how drunk I got, just so long as they didn’t have to physically carry me home.
For me, learning to live a sober life has been like trying to walk when you’re used to crawling.
It’s been two-and-a-half years, but I still remember how easy it was to drink, and it’s taken a lot of effort for me to reach an emotional place where I’m strong enough to choose another option.
The hardest part of sobriety has been learning to be comfortable with myself all the time. Every day, it gets a little easier. But I’ve had to teach myself how to communicate thoughtfully without poisoning my speech with the fury of alcohol. I’ve had to learn how to flirt and pursue romance without being a histrionic drunk, lacking both grace and inhibitions.
I understand I have a long way to travel before I achieve self-acceptance or real serenity.
But what I do have, finally, is the peace of mind of knowing that I can wake up every morning remembering what I did the night before — for better or worse — and knowing, in the end, that I will be OK.