Family Shares Embarrassing Perm Photos To Help Autistic Son
When you go to the doctor, you want the latest, greatest treatment. If you have decent insurance, you expect them to cover something that's at least pretty good.
So you can imagine this mom's shock when her insurer told her that the only treatment options for her son, who has autism — treatments that had worked for him in the past — would not be covered based on scientific opinions popular in the 1970s.
Lots of children with autism benefit from applied behavior analysis (ABA) therapy. For some, it's the only treatment that works. But many insurers don't cover it, citing research from an era before personal computers. Or Justin Timberlake. Or disposable contact lenses.
ABA, this miracle therapy, is crazy expensive. It can cost up to $50,000 per year. (But don't let sticker shock freak you out, retronauts — DollarTimes tells us that's only $8,088.43 in 1970's dollars.)
(Apparently smocking was a thing in the '70s.)
I learned about this because of a kid named Martin. Martin is a nice kid. He re-creates OK Go videos in Lego and could tell you everything you never wanted to know about every single U.S. president. He just has a bit of trouble with social situations. Sometimes more than a bit.
When he was 4, he did some intensive ABA therapy. It taught him how to talk. It taught him how to use the toilet. It helped him do all sorts of everyday things, from putting on clothes to trick-or-treating.
Years later, he needs some more intensive treatment. Social stuff is getting more complicated as he heads toward the hormonal toxic waste dump that is middle school. In his frustration, Martin began to act out. He threw fits. He started hitting his teachers and family members. His parents decided to see if they could get him back into ABA. It worked a miracle before, and although it was once controversial, it's now accepted as best practice for many people with autism. Martin's parents are well-insured. They both work for the University of Texas at Austin.
But their insurance won't cover the therapy that worked for him in the past. Rather than trust recent studies that show ABA's effectiveness, the insurers doubt the science and reflect skeptical attitudes about ABA from the 1970s.
You remember the 1970s, right? Back when polyester was in, disco was hopping, and gas was leaded?
Martin's mom, Dr. Jennifer Graber, got super pissed off. She's been fighting for him for a long time now, and she has had enough.
The law in Texas actually requires insurers to cover ABA, but UT is exempt. The reasons are complicated, but that's how our insurance system goes. Loopholes and fine print everywhere.
And you know what? Your insurance very well might not cover ABA either. Many states don't require it. You might not find out what you don't have until you desperately need it. Or your friend does. Or your grandkid.
According to Autism Speaks, many states have tried to pass legislation to require insurers to cover ABA. But even within states, like Texas, that have passed reform legislation, loopholes allow large institutions to avoid coverage. There are also several states where efforts to pass reform measures have not succeeded and others in which no reform legislation has been brought forward. There are thousands of children with autism in the U.S. with no affordable access to ABA therapy.
It's time to exit the 1970s. Martin's mom has started a petition to hassle the folks at UT about their retrograde policies, as well as a hilarious/depressing/hilarious Facebook page where people are sharing their reasons the 1970s were, as decades go, suboptimal. You can add your own awkward '70s photos and sign their petition.
I'd like to propose a bigger action. Check out the law related to insurance coverage of autism in your state and if it stinks, write your representatives. You might not have a person with autism in your life right now, but statistically, it's only a matter of time before this hits home.
UPDATE:
Good news! After Dr. Graber's petition got a bunch of signatures, the University of Texas announced that it will begin covering ABA therapy for children with autism in fall 2015! But there are unfortunately still many children with different insurance who don't have access.



 Each of those arms has its own brain?
Each of those arms has its own brain?
 Homemade granola bars with chocolate chips – perfect for a delicious snack!
Homemade granola bars with chocolate chips – perfect for a delicious snack! Refresh with a healthy green juice boost.
Refresh with a healthy green juice boost. Making fresh orange juice in the kitchen. 🍊
Making fresh orange juice in the kitchen. 🍊 Be careful with supplements.
Be careful with supplements.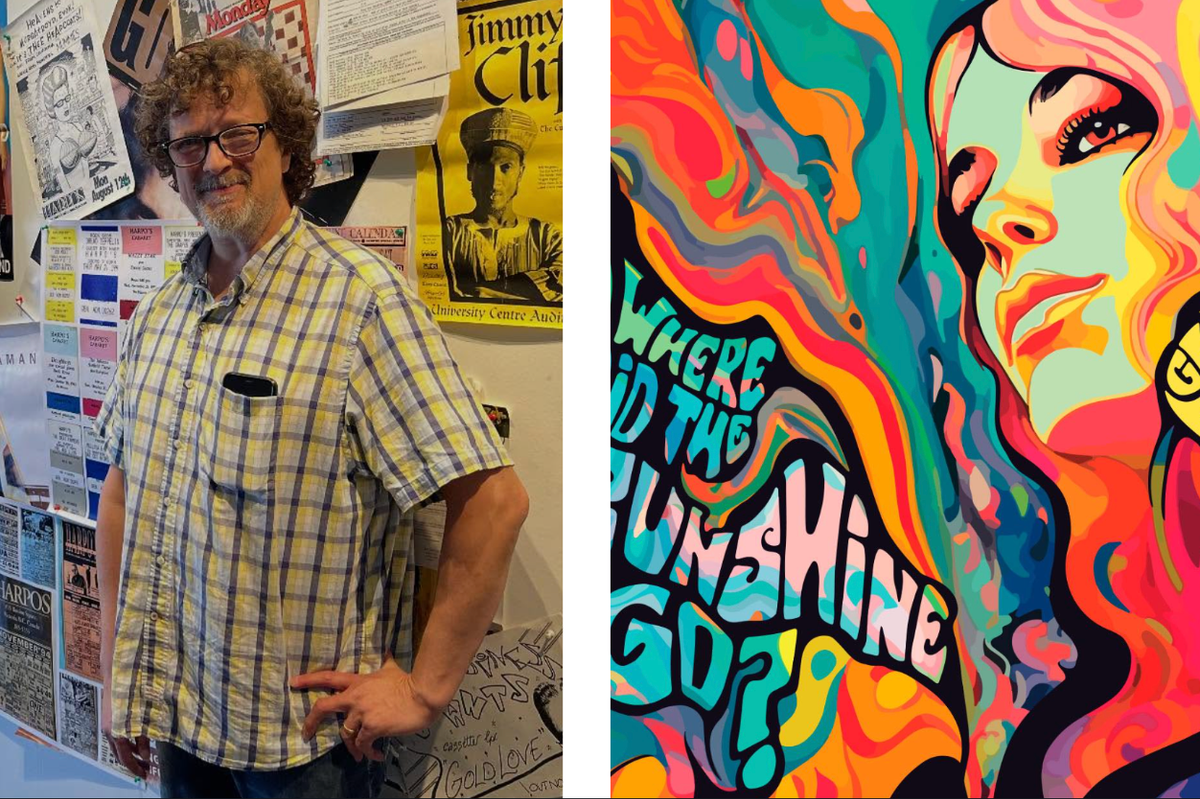

 A white porcelain doll with a tear stain. Photo by
A white porcelain doll with a tear stain. Photo by 