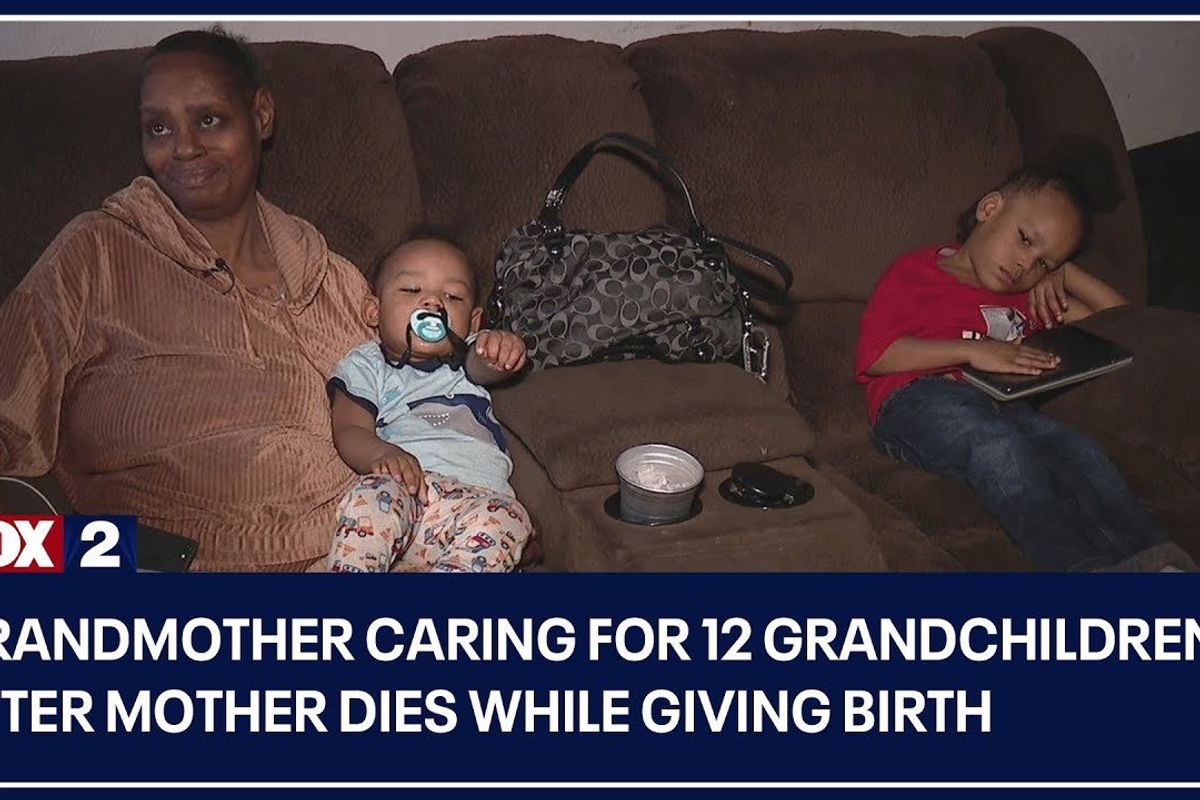
People rallied to support grandmother raising 12 children after their mother died giving birth
The grandmother hopes that no other parent has to experience this tragedy.
People help support grandmother raising 12 grandchildren.
When most people have children, they hope that their own parents will be around to watch them grow up. They're not often thinking about their own mortality at that stage of life. But sadly, sometimes parents are the ones that don't get to watch their children grow up, and it's the grandparents tasked with raising their grandchildren.
Patricia Pouncey is one of those grandparents left caring for her grandchildren after her daughter, Nikita Washington, gave birth to her 12th child on December 22. Washington went into Harper University Hospital in Detroit due to high blood pressure before requiring a cesarean section, according to ABC12. The 35-year-old was at the hospital alone as her mother was caring for her other children and her husband is currently incarcerated.
But after learning of the cesarean, her family did not hear from her again, which prompted her sister to go to the hospital to check on Washington. This is when the family discovered that the mother of 12 had passed away after complications from the surgery.
With Washington's husband in jail, Pouncey is left as the sole caregiver of the children, now aged 3 months to 19 years old. Taking on a child without warning is a lot to handle, but taking in 12 grieving children while you are also grieving has to feel nearly impossible. But Pouncey has been doing whatever she can to make sure the children continue to stay together in her home, and others have been pitching in to help.

Woman in black-and-white striped shirt carrying baby in white onesie with rocket ships on it.
Photo by Lawrence Crayton on UnsplashWashington's sister Daveia Knox started a GoFundMe to help with funeral expenses and to assist Pouncey with money to raise the children. So far, the account has raised more than $104K and helped the grandmother purchase a more reliable vehicle and a larger home to house all of the children. The comments on the GoFundMe have been extremely supportive of the grieving family.
"May God strengthen you & bless you with much prosperity to raise your grandchildren without lacking anything! I’m extremely sorry for your loss & pray you got the answers you need. Blessings," wrote one donor.
"This was such an unexpected tragedy, the generosity & sacrifice of grandma, and to care for the children. May God bless the family and all those who donate in any way they can: money, food, childcare, etc.," another donor wrote.
There have been donors giving donations of all sizes, from $5 to $3,000, hoping to help the grandma care for her dozen grandchildren. Surely each donation is appreciated and will be used for things like groceries, baby formula, clothing, shoes and other things required to raise children.
Pouncey hasn't received information on what happened to her daughter while at the hospital that led to her death.
"I haven't talked to anyone from the hospital. I have not received anything from them. All I have is the death certificate," the grandmother told CNN.
"If she died naturally, I want to know. If one of them doctors did something, I wanna know that too," Pouncey told Fox 2 Detroit. "I'm hurt, I'm confused."
Currently, Black maternal mortality is 2.6 times higher than that of white women, and Black infants are more than twice as likely to die after birth than white infants. Unfortunately, Washington became one of the Black women who make up the statistic, and Pouncey is hoping no other mother has to go through what she is going through.
"I'm worried about every mother," Pouncey told CNN. "Don't ever, ever make the mistake that I made, letting your child go (to the hospital) alone. We need to give more attention to what's going on."
April 11 to 17, 2023 was Black Maternal Health Week, during which events and campaigns were held to raise awareness around Black maternal mortality rates. The annual week also focuses on programs and initiatives to support Black mothers.
If you'd like to donate to support the family, you can find their GoFundMe here.
This article originally appeared on 4.18.23
- COVID-19 has made the overlooked Black maternal health crisis even more vital to address ›
- Mom sparks passionate debate after saying she would choose her own life over child’s during birth ›
- 2 dads are on a mission to end Black maternal mortality after losing ... ›
- Grandma's laugh after getting hair colored is infectious - Upworthy ›