When I was a kid, I went on a lot of nature walks with my mom.
We lived in the country in Central Texas and had a little plot of woods all to ourselves. We walked around big, ancient oaks and twisted, gnarly mesquite trees. Sometimes, we'd find a tree covered in big, ropey mustang grapevines and I'd climb up into the trees, pretending I was in the Swiss Family Robinson.
Other times, we went looking for animals. My favorites were the green anole lizards that lived on trees and flashed their red neck flaps at you.
Technically, it's called a dewlap, thank you very much. Photo from R. Colin Blenis/Wikimedia Commons.
There were also tiny black-and-white beetles with rock-hard shells that lived on fallen logs. If you touched them, they played dead until they thought you were gone. And sometimes we even saw deer.
Nature walks are a good way for families to bond. And they're pretty healthy too.
Science shows that spending just a little time outside (walking, looking at the trees, or even catching Pokemon!) can be good for you — it reduces blood pressure and improves mental health. There are even studies that suggest spending time in nature together can help families get along.
But here's the problem: Not everyone has access to nature, even (and especially) in rural areas.
Does this count as nature? Not really. Scott Olsen/Getty Images.
It's easy to imagine how someone living in downtown Chicago might struggle to find nature. But living outside a city doesn't guarantee access to trails and forests, either.
For example, imagine living in farm country. Though you're definitely not in the city, miles and miles of corn fields are just as much an artificial creation as any apartment building (plus the farmers probably wouldn't be happy with you trying to picnic in the middle of their fields).
This is actually a significant problem, so two researchers (University of Illinois professor Ramona Oswald and doctoral student Dina Izenstark) recently examined the lack of nature access in rural America. They found that although a lot of parents may know how great a nature walk can be for both your mood and your body, long distances or costs keep them from getting their families into nature.
“The moms in this study know about health and what to do to be healthy,” Oswald said in a press release. “It’s not a lack of education. It has to do with barriers and access to resources."
But what if we could erase these barriers? Enter the Rails-to-Trails Conservancy, a nonprofit that's giving people access to nature in a cool way: by reviving old railway lines.
Photo via Rails-to-Trails Conservancy/Eric Oberg, used with permission.
You see, the United States is criss-crossed with old railway lines.
Photo via iStock.
Many of them are still in use, but many have been abandoned.
Photo via iStock.
But just because they're abandoned doesn't mean they can't still be useful.
These abandoned lines can have new life breathed into them. Take the Cardinal Greenway in central and eastern Indiana.
Way back in 1993, the nonprofit Cardinal Greenways bought 60 miles of abandoned railroad in eastern Indiana and, after teaming up with the Rails-to-Trails Conservancy for logistical help, began the hard work of turning it into a nature trail. (Rails-to-Trails support projects all across the United States.)
Photo from Cardinal Greenways, used with permission.
Tearing up a big metal railroad to make a nature trail might seem like a lot of work. But the railroad is already set up for nature walking success.
Most railroad tracks are already built up off the ground (so they don't flood), and they can support a lot of weight. Even better, trees don't grow on railroad tracks, so there's less vegetation to cut back to make a trail.
Cardinal Greenways' first 10-mile stretch opened in 1998.
They also added updated features like new bridges, benches, and informational signs.
Photo from Cardinal Greenways, used with permission.
There is also a playground and exercise equipment. You can even borrow a bike. It's free, too. Cardinal Greenways relies on volunteers and donations to maintain and expand the trail.
Today, the Cardinal Greenway runs for 62 miles, winding through more than 10 small towns as well as nature preserves and parks.
Photo from Cardinal Greenways, used with permission.
Families can walk or bicycle it, giving them easy access to nature and a safe place to exercise, no matter whether they're urban or rural.
A lot of different places have hit on replacing old railway lines with nature trails. Chicagoans might recognize the Bloomingdale Trail, for instance.
Photo from Victor Grigas/Wikimedia Commons.
The Bloomingdale Trail is a greenway that runs for about three miles in Northwest Chicago. You might never guess it used to be an old elevated train line.
In fact, your favorite running trail may have started its life as a railroad track. The Gloucester Township Trail in New Jersey, the Shelby Farms Greenline in Tennessee, and Mississippi's Tanglefoot Trail all started as old train lines, too.
Projects like this give both urban and rural families access to nature — using resources we already have.
Nature walks with my mom are some of my fondest childhood memories, and I'm sure those walks are part of the reason I'm still in love with nature today.
It's awesome to see projects like this making sure everyone has access to those memories like I did.







 Many people make bucket lists of things they want in life.
Many people make bucket lists of things they want in life. 
 The Challenger on crawler transport
The Challenger on crawler transport The Challenger explosion.
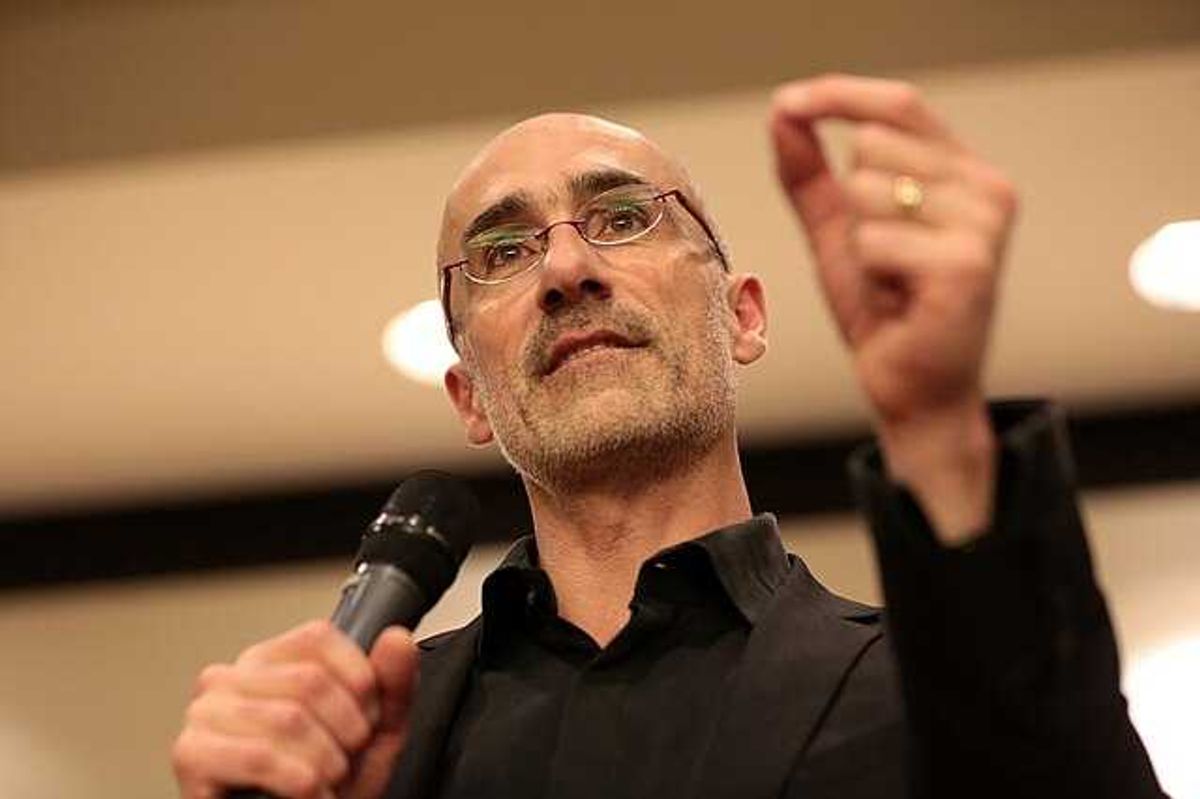
The Challenger explosion.  Jay Greene in the control room after the Challenger explodes
Jay Greene in the control room after the Challenger explodes
 sipping modern family GIF
sipping modern family GIF 
 A woman is getting angry at her coworker.via
A woman is getting angry at her coworker.via  A man with tape over his mouth.via
A man with tape over his mouth.via  A husband is angry with his wife. via
A husband is angry with his wife. via 
 Two kids enjoying a video game together on the couch. 🎮✨
Two kids enjoying a video game together on the couch. 🎮✨ Family gaming fun: everyone is focused and competitive!
Family gaming fun: everyone is focused and competitive!