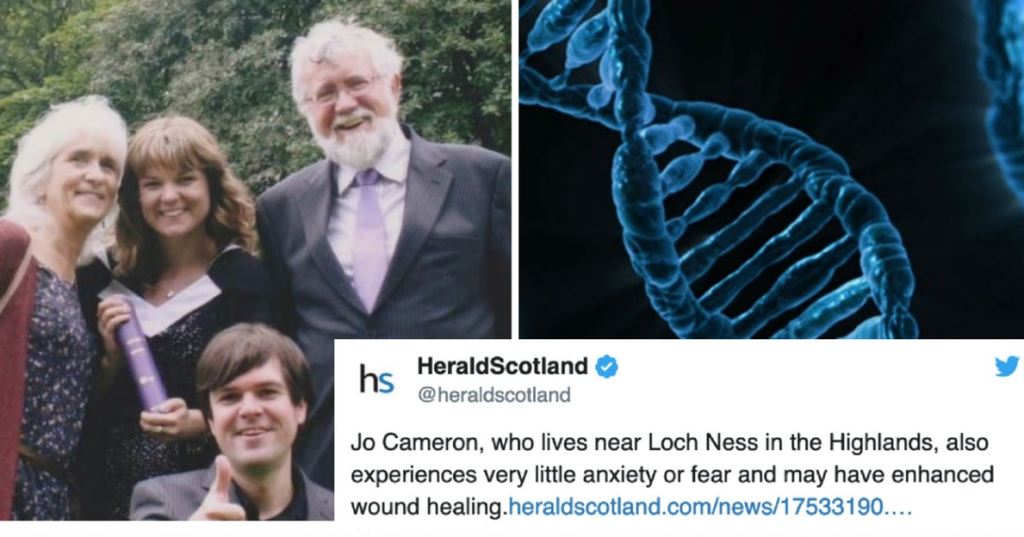
Jo Cameron has been pain-free all her life — something many might dub a superpower of sorts.
While other women struggle with the pain that comes along with childbirth, when Cameron gave birth to her two children, she felt only “a tickle.” Later on in life, she didn’t realize she needed to have her hip replaced until she physically couldn’t walk. She also couldn’t tell she had been burned until others smelled burning flesh, and failed to notice cuts until someone else pointed out blood. Spicy foods — such as Scotch bonnet chili peppers — didn’t set her mouth on fire and instead left her with a “pleasant glow.”
Her body also heals more quickly than most, with her injuries rarely resulting in scars.
[rebelmouse-image 19534995 dam=1 original_size=”640×426″ caption=”Image by Hans/Pixabay.” expand=1]
While all this sounds pretty incredible, Cameron didn’t think much of it until around five years ago, after she underwent surgery on her hand. She told her doctor, Dr. Devjit Srivastava, that she wouldn’t need any pain medication during recovery. Obviously, this was an unusual patient request, but after delving into her medical history, he quickly realized she was a special case.
So he sent her to see a team of doctors and researchers focused on how genetics can be used to understand the biology of pain and touch at the University College London’s Molecular Nociception Group. Eventually they wrote a paper, which was published on Thursday in The British Journal of Anaesthesia, on the curious case of Cameron, whose pain-free existence seemed unexplainable.
Though these specialists had worked with several individuals who process pain differently, Cameron’s genetic profile was unique for an individual who couldn’t feel pain.
Eventually they discovered her uniqueness could be explained by the fact that she is missing the front of a gene they have dubbed FAAH-OUT — a gene all us have — but they claim she is the only individual they know about who has this specific genetic mutation.
[rebelmouse-image 19534996 dam=1 original_size=”640×360″ caption=”Image by Public Domain/Pixabay.” expand=1]
“We’ve never come across a patient like this,” John Wood, the head of the Molecular Nociception Group at University College London, revealed to the New York Times.
According to researchers, this mutated gene does more than prevents Cameron from feeling pain. She also can’t feel fear or anxiety, which doctors think have something to do with the gene mutation making her more forgetful.
“It’s called the happy gene or forgetful gene. I have been annoying people by being happy and forgetful all my life – I’ve got an excuse now,” she told the BBC.
Jo Cameron believes she inherited the mutation from her late father, who she remembers suffered from little pain as well.
“I can’t remember him needing any painkillers,” she told the New York Times. “I think that’s why I didn’t find it odd.” Since he is no longer living, there is no way to know if he was a carrier. While her daughter and mother do not have the mutation, according to her doctors, her son “has the same microdeletion in FAAH-OUT, but does not have the other mutation that confers reduced FAAH function.” So he’s insensitive to some pain, but not all.
Could Cameron’s extraordinary gene help others manage their pain and anxiety better? Doctors are hopeful, but the road ahead is long.
Researchers hope that further studies will help them design gene therapy, pain intervention methods or anxiety medications, though expect it will take many years and a lot of money before a product will emerge.
“I’m reasonably confident that the lessons we are learning from the genes involved in pain will lead to the development of an entirely new class of pain medications,” Dr. Stephen G. Waxman, a Yale neurologist who was not involved with the paper but has studied the subject matter, told the New York Times.
[rebelmouse-image 19534997 dam=1 original_size=”640×426″ caption=”Image by Steve Buissinne/Pixabay” expand=1]
Considering that painkillers on the market today — especially opioids like oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine and morphine — are incredibly addictive and responsible for tens of thousands of drug overdoses every year, finding a responsible pain cure could save so many lives. And if there are more people like Cameron out there, the likelihood of this mutation resulting in a novel pain treatment system is even higher.
There are lots of unknowns, but scientists have come a long way in their research with genetics in recent years. It will be exciting to see the impact an unusual case like Cameron’s has on medicine in the years to come.