9 risk factors for suicide and 1 important question you can ask to hopefully know for sure.
There's something you should know about people with severe depression.
Many of us feel inept when it comes to acknowledging suicide.
"It's so tragic."
"What a waste of a beautiful life."
"Why didn't he just talk to us about it?"
We are often at a loss for how to deal with the profoundly devastating topic of suicide. We can talk about it in a removed, social-ill, this-world-is-so-messed-up, throw-our-hands-up-in-helplessness kind of way when it comes up in passing — like when people are talking about how much they miss Robin Williams.
But we are poorly equipped to discuss it in any substantial way. Which is understandable. Most of us aren't trained in psychiatric services and are doing our best to muddle through our own difficulties in life. Figuring out how to solve America's suicide problem seems above our pay grade.
It's important for each of us to commit to getting better at talking about it.
When you have that one friend you can just sit and talk with about anything. Image by Garry Knight/Flickr.
The truth is that each of us could have a friend who's suicidal right now — today — and isn't telling us about it. They're not telling us about it because they know very well that they live in a world ill-equipped to help them without judging them.
The main thing that kept me from speaking up long ago when I toyed with the thought of ending my own life was: "If I admit I'm barely able to take each next breath right now, will I always be labeled as fragile or troubled forever for the rest of time?" Saying something is a decision to commit to someone else's memory that this messed-up mental stumble is happening. It takes bravery to talk about it, especially when you're in the thick of it.
Everyone and anyone could be at risk for suicide. Suicide doesn't have a "look." Moms, dads, 11-year-olds, pastors — the thought of ending it all can take root in anybody's mind. But there are some groups who are more prone to suicide than others. According to the CDC, lesbian, gay, and bisexual youth are four times more likely to attempt suicide than straight peers. And 25% of transgender young people surveyed report having made an attempt to take their own life. The thing that some well-meaning people don't know is that snapping out of it or learning how to enjoy life isn't an option for those who are truly depressed — it's not a mind-over-matter thing. At that particular moment in their lives, the afflicted person just can't.
The little things that can spark our spirit during normal times don't do the same thing for someone who's depressed. Image by Rick/Flickr.
Why does suicide start looking like a viable option?
John Gibson, a pastor whose name was recently released as part of the Ashley Madison hack (where people were outed for starting accounts with the intent to cheat on their spouses), committed suicide in August.
"He talked about depression. He talked about having his name on there, and he said he was just very, very sorry. What we know about him is that he poured his life into other people, and he offered grace and mercy and forgiveness to everyone else, but somehow he couldn't extend that to himself."
— Christi Gibson, on her husband John's suicide letter
Jody Nelson, a clinical social worker in Lansing, Michigan, explains part of why a person can be drawn to suicide in the first place:
"A suicidal person will often see suicide as a neat, tidy, and self-contained solution to their emotional state of desperation. Suicide is never neat. Never tidy. And never truly self-contained. Suicidal people are not capable of seeing or predicting the ripples and waves their act will cause in lives around them. Yet their suicide will impact lives they aren't even aware they are touching via connections their own illness makes impossible for them to see."
He advises us to know the risk factors:
"Not all of these are going to mean impending suicide attempts, but the risk increases as they pile on each other."
1. Depression. Isolation. Losses.
2. Big life changes (and sometimes, just some small ones like going on or off certain meds).
3. Prior attempts. Substance abuse.
4. Irrational or erratic behaviors.
5. Financial difficulties.
6. Access to means.
7. Suicidal intention.
8. A family history of suicide.
9. Connections to others who have died by suicide.
Nelson says that if we see those signs, we should ask straight-up something like this question:
"Hey I've noticed you've been particularly down lately. Are you thinking about hurting yourself?"
It won't make someone who's not suicidal suddenly consider it. And it won't make someone who is thinking suicidal thoughts go through with it. What it will do, if they have been thinking about it, is break through a wall that's keeping the person isolated and suddenly alleviate some of that buildup they've been sitting alone with. A person struggling with depression and suicidal thoughts is often very grateful to find someone they can talk frankly with about their thoughts.
And if they say yes, listen and talk, but also get them to an emergency room. Go with them. Get them there. They will be connected to the right resources once they get there. Then follow up and keep an eye. Keep talking with them. But don't let them put it off — they will try to downplay it as not that serious. Who wouldn't?
Here's why it's important for us to talk about this right now, and publicly.
There's no shame in needing your friends. These guys know. Image by SmellyAvocado.
When we learn how to talk about suicide more productively and demonstrate publicly that we're trying to understand it a little better than we used to, we open doors in case someone in our circle is thinking about opening up.
We signal that we aren't going to judge our friends and loved ones — just love them. Sharing an article like this is one way to start sending that signal.
And when more people get the message that there's someone around they can talk to, maybe we'll see the suicide numbers drop significantly.
In the big picture, that would be amazing. But as anyone who's lost a loved one to suicide can tell you, saving one person and stopping those devastating ripple effects from starting is immeasurably valuable.




 Curtains can help make a space feel homey and hide bad windows and trim.
Curtains can help make a space feel homey and hide bad windows and trim. Clean and tidy sets a mood.
Clean and tidy sets a mood. Lighting makes a big difference in how your home feels.
Lighting makes a big difference in how your home feels.
 A man being licked by a golden retreiver.
A man being licked by a golden retreiver.  A dog's tongue close-up.
A dog's tongue close-up.  A golden retreiver getting their teeth brushed.
A golden retreiver getting their teeth brushed. 
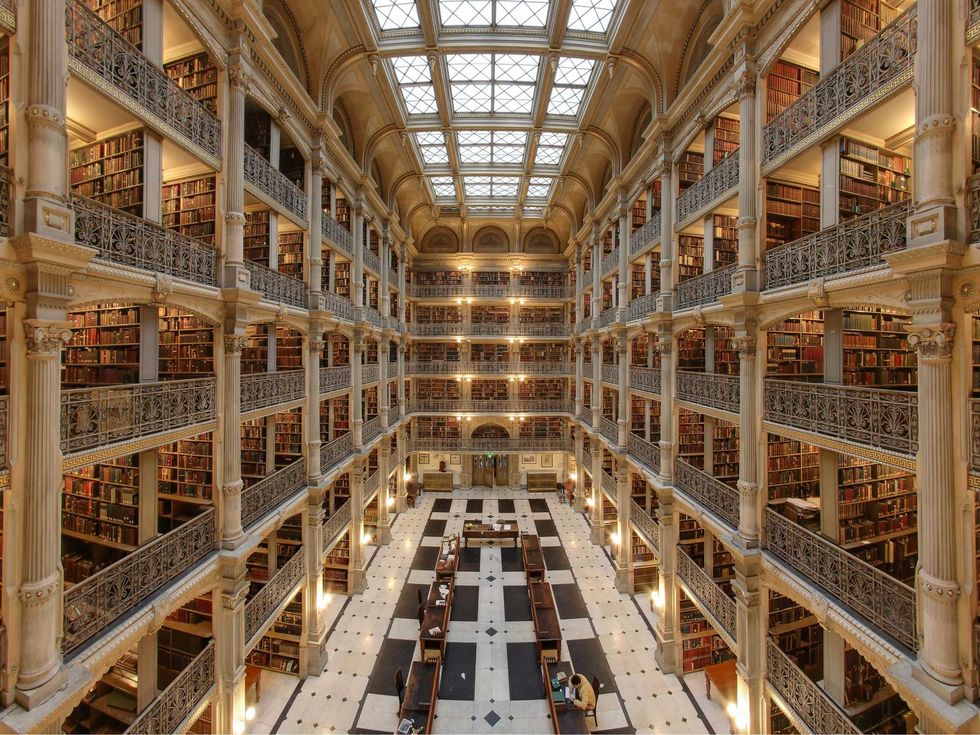 Cathedral-like libraries like the George Peabody Library in Baltimore, Maryland are popular places for creative work.By Matthew Petroff/
Cathedral-like libraries like the George Peabody Library in Baltimore, Maryland are popular places for creative work.By Matthew Petroff/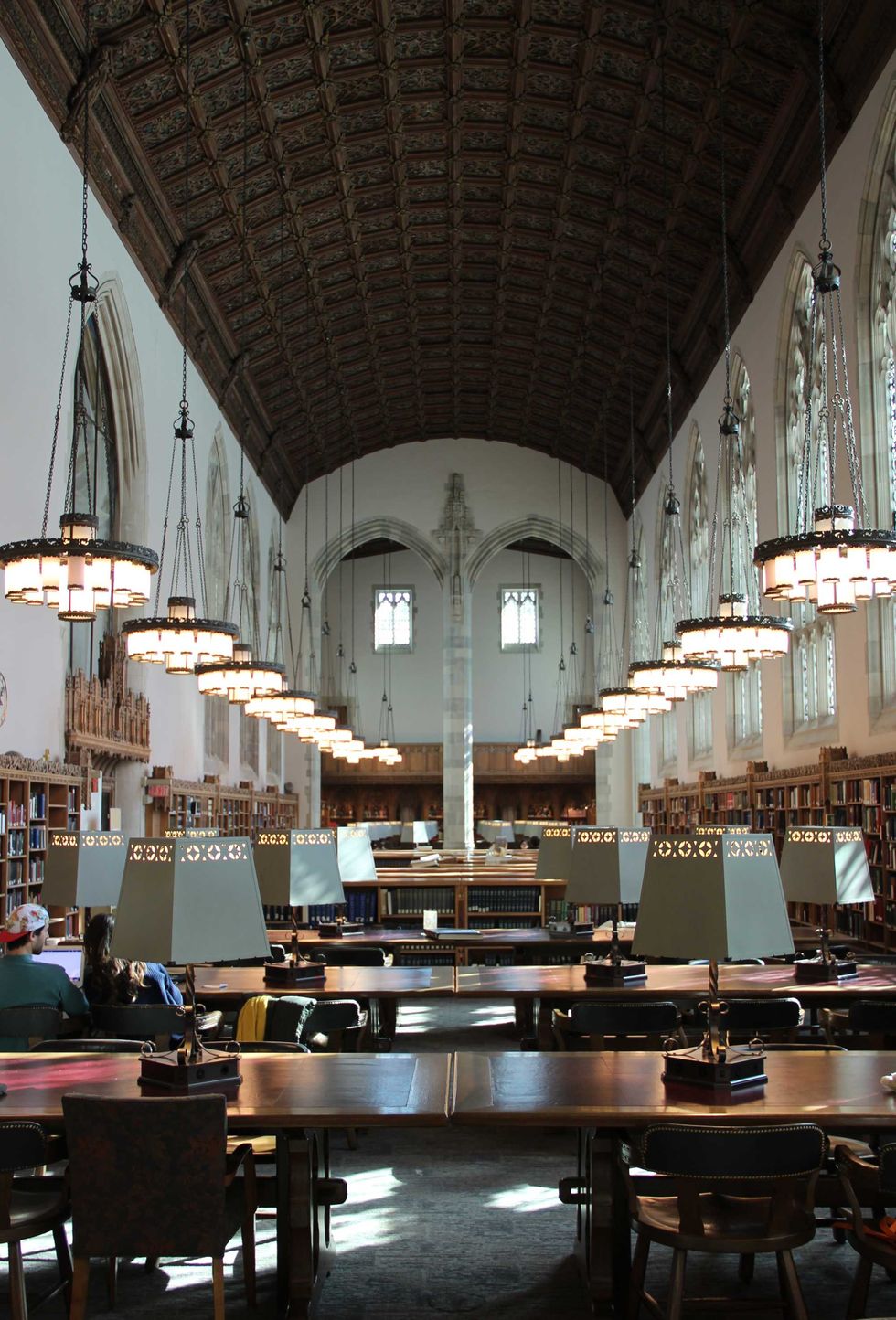 The Sterling Memorial Library at YaleBy Nick Allen/
The Sterling Memorial Library at YaleBy Nick Allen/
 A woman making eye contact with a man she is speaking to.via
A woman making eye contact with a man she is speaking to.via  A man in a suit with questions.via
A man in a suit with questions.via