13 usually unspoken tips if your loved one struggles with depression.
If you love a person who has depression, you'll want to remember these things.
1. Depression is not a choice.
Depression is one of the most helpless and frustrating experiences a person can have. It’s sometimes feeling sad, sometimes feeling empty, and sometimes feeling absolutely nothing at all. There are times when depression can leave someone feeling paralyzed in their own mind and body, unable to do the things they used to love to do or the things they know they should be doing. Depression is not just a bad day or a bad mood, and it’s not something someone can just “get over.” Remember: No one chooses to be depressed.
Photo via iStock.
2. Saying things like “it’ll get better,” “you just need to get out of the house,” or “you’ll be fine” doesn't help.
It’s easy to tell someone these things because you think you’re giving them a solution or a simple way to make them feel better and ease their pain. But these kinds of phrases almost always come across as empty, insulting, and essentially meaningless.
In fact, saying these phrases only creates more tension within, making people feel as though they’re inadequate, and like you’re not acknowledging what they’re going through by trying to put a Band-Aid on a much larger issue. They understand you’re just trying to help, but these words will only make them feel worse. A silent hug can do so much more than using cliched sayings. What you can say instead:
"I’m here for you. I believe in you. I believe you are stronger than this, and I believe you’ll get through this. What can I do to help you? What do you think would make you feel better?"
Avoid offering advice, but instead just let them know you’re there for them and ask them questions to help guide them in discovering what could make them feel better.
3. Sometimes they have to push you away before they can bring you closer.
People who suffer from depression often get frustrated with feeling like they’re a burden on other people. This causes them to isolate themselves and push away people they need the most, mentally exhausting themselves from worrying about whether they’re weighing down their loved ones with their sadness. If they become distant, just remember to let them know you’re still there, but don’t try to force them to hang out or talk about what’s going on if they don’t want to.
4. You’re allowed to get frustrated.
Just because someone deals with depression doesn’t mean you have to cater to all of their needs or walk on eggshells when you’re around them. Depressed people need to feel loved and supported, but if it begins to negatively affect your life, you’re also allowed to acknowledge this and figure out how to show them love and kindness without self-sacrificing.
Photo via iStock.
5. It’s important to discuss and create boundaries.
In those moments of frustration, it’s important to take a step back and look at how you can help the depressed person while also maintaining your own sense of happiness and fulfillment. Be patient. Talk to them about your concerns and explain the boundaries you need to create within your relationship. Find out something that works for both of you.
6. They can become easily overwhelmed.
Constant exhaustion is a common side effect of depression. Just getting through the day can be an overwhelming and exhausting experience. They may seem and look totally fine one moment, but in the next moment feel tired and have no energy at all, even if they’re getting plenty of sleep every night. This can result in canceling plans suddenly, leaving events early, or saying no to things altogether. Just remember that it’s not about anything you did. It’s just one of the prevalent side effects of living with the disease.
7. It’s not about you.
When you have a loved one dealing with depression, it can be difficult to understand what they’re going through and to consider how their sadness is a reflection of your relationship with them. If they need space or become distant, don’t blame yourself and wonder how you could do things differently to heal them. Understand their depression is not about you.
8. Avoid creating ultimatums, making demands, or using a “tough-love” approach.
Telling someone that you’re going to break up with them or not talk to them anymore if they don’t get better is not going to magically cure them of their illness. They won’t suddenly become the person you want them to be just because you’re tired of dealing with their problems. It’s a personal decision to walk away from someone if their issues become too much for you and your relationship with them, but thinking the "tough-love" approach will make them better is unrealistic and manipulative.
9. They don’t always want to do this alone.
It's easy to assume people dealing with depression want to just be left alone. While there may be times when they want their space, that doesn’t mean they want to face their fears alone. Offer to take them on a drive somewhere. Ask if they want to get coffee or a meal. One-on-one time when you can bring them out of their routine and connect with them can mean everything to them.
Photo via iStock.
Reach out to them unexpectedly. Remind them they don’t have to do this alone.
10. Try not to compare your experiences with theirs.
When someone is going through a rough time, we often want to share our own stories with them to let them know we've gone through something similar and can relate with their struggle. When you say something like, “Oh yeah, this one time I was depressed too...” it only makes them feel like you’re minimizing their pain. Express empathy, but don’t suppress their feelings. The greatest resource you can share with your friend is your ability to listen. That’s all they really need.
11. It’s OK to ask your friend where they are in their feelings.
How are they really feeling, and how are they coping with their depression? Suicidal thoughts are a common occurrence for depressed people. It’s OK to directly ask them how they're practicing self-care and to come up with a safety plan for times when their depression becomes too overwhelming.
12. Schedule time to spend together.
Offer to spend time with them once or twice a week to exercise, shop, or hang out together. Ask if you can cook dinner with them and plan a friend date.
Photo via iStock.
One of the hardest parts of depression is feeling too exhausted to cook healthy meals, so you can really help them out by cooking food they can store in their fridge or freezer for later.
13. Just because someone is depressed doesn’t mean they’re weak.
In his book "Against Happiness: In Praise of Melancholia," author Eric G. Wilson explores the depths of sadness and how experiencing mental anguish can actually make us more empathetic, creative people. Although he explains the difference between depression and melancholia, he rejects the idea of inflated happiness that our culture and society is obsessed with and instead explains why we reap benefits from the darker moments in life.
Wilson writes:
“I for one am afraid that our American culture’s overemphasis on happiness at the expense of sadness might be dangerous, a wanton forgetting of an essential part of a full life. I further am wary in the face of this possibility: to desire only happiness in a world undoubtedly tragic is to become inauthentic, to settle for unrealistic abstractions that ignore concrete situations. I am finally fearful over our society’s efforts to expunge melancholia from the system. Without the agitations of the soul, would all of our magnificently yearning towers topple? Would our heart-torn symphonies cease?”
In a similar manner, psychiatrist and philosopher Dr. Neel Burton discusses in his TEDx Talk that some of the most influential and important people in history have experienced depression. He explains the way our culture looks at and treats depression, and how traditional societies differed in their approach, seeing human distress as an indicator of the need to address important life problems, not a mental illness.
It’s important to remember depression is not something that should be considered shameful, and experiencing it doesn’t make someone weak or inadequate.




 Corgi cuddles spreading joy and smiles!
Corgi cuddles spreading joy and smiles! Joyful moments with furry friends! 🐶❤️
Joyful moments with furry friends! 🐶❤️

 Cat sitting in a woman's lap
Cat sitting in a woman's lap Cat making biscuits
Cat making biscuits Who knew yawning and stretching could be a sign of love?
Who knew yawning and stretching could be a sign of love?
 An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant. 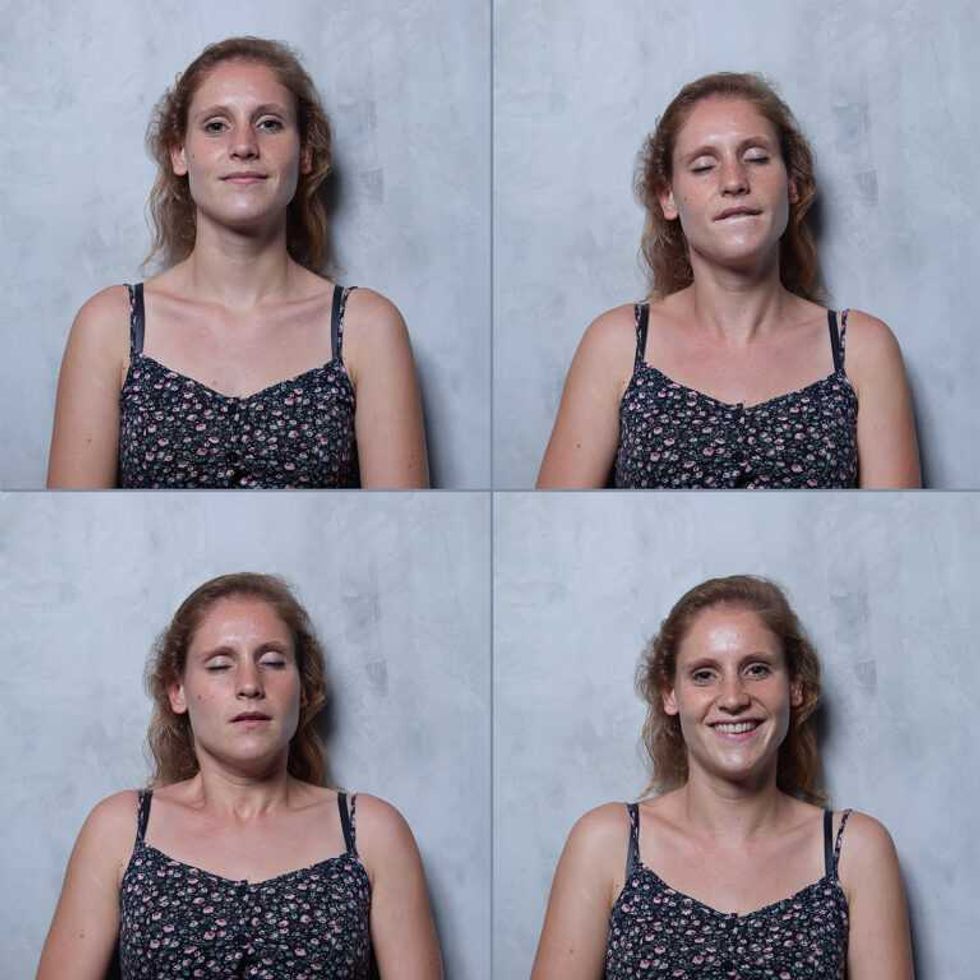 An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant. 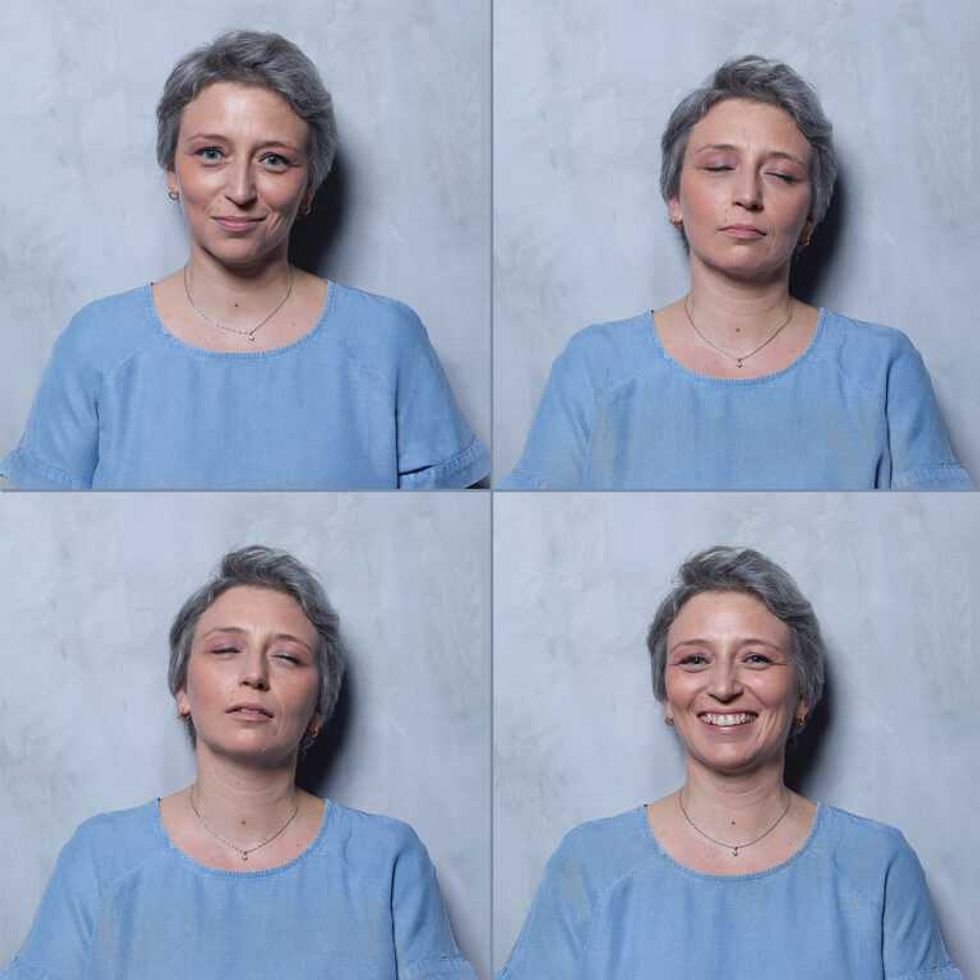 An O Project participant.
An O Project participant.  An O Project participant.
An O Project participant.