Dr. Anthony Fauci remembers the first AIDS patient he ever met.
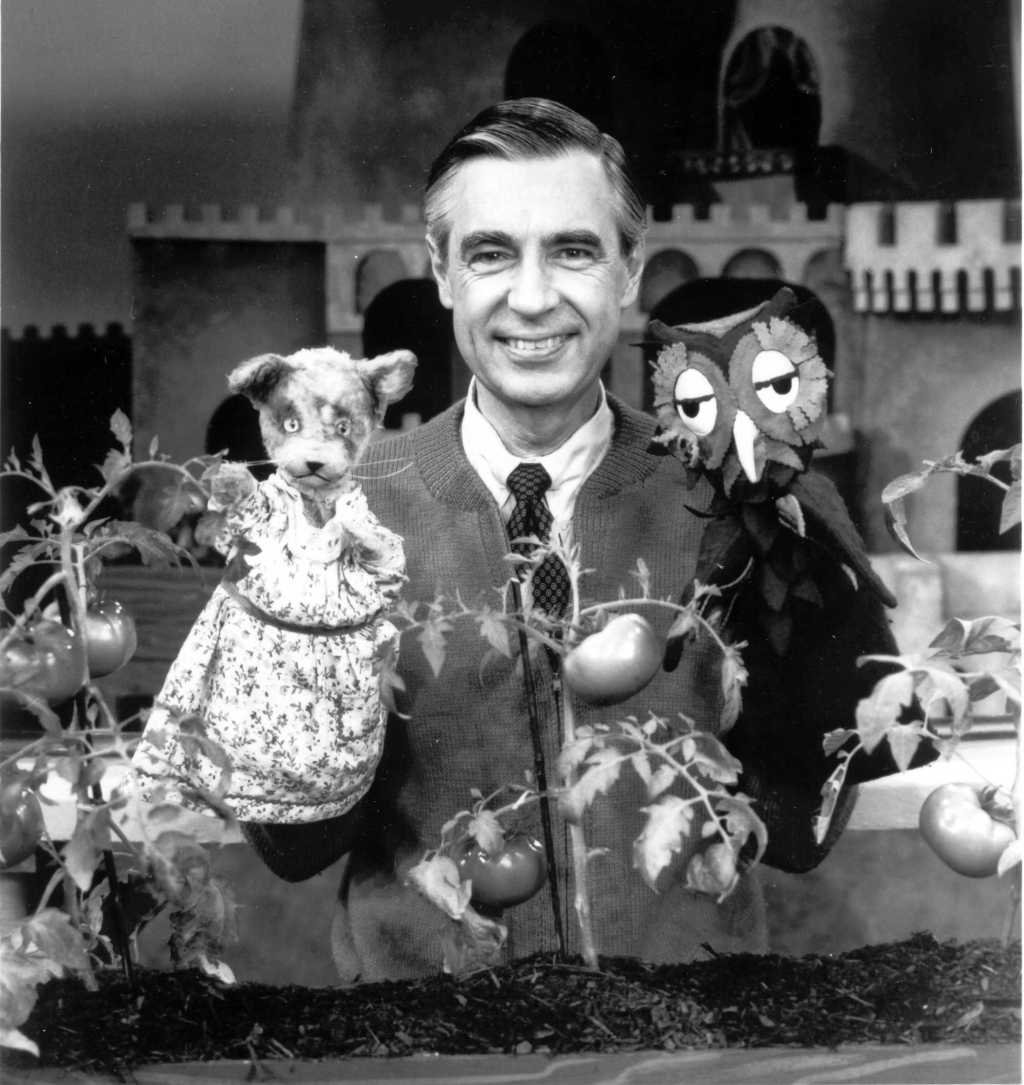
Fauci at a conference in 2015. Photo from Bluerasberry/Wikimedia Commons.
It was 1981. A young man walked into Fauci’s office. He was very sick and getting worse. Among his other maladies, an opportunistic infection was attacking his retinas — the man was going blind right in front of Fauci. But there wasn’t anything Fauci could do for him.
At the time, doctors didn’t even know what AIDS was. It would be a year before the term was even invented.
“It was a very painful and very frustrating because, you know, when you’re a physician you’re trained as a healer,” said Fauci. But he couldn’t heal this young man. The patient eventually died of the disease.
“That was the first of several thousand patients I’ve seen over the last 35 years,” Fauci said.
But Fauci didn’t give up.
Now, more than 30 years after Fauci met that patient, we may be well on the way to stopping AIDS, thanks to a new vaccine.
Photo from Mujahid Safodien/AFP/Getty Images.
Today, Fauci is the director of the National Institute of Allergy and Infectious Diseases (NIAID). They work to treat and prevent a wide range of diseases, including HIV/AIDS.
Thanks to the work of the NIAID and a whole host of other doctors, scientists, and organizations, our relationship to HIV/AIDS has completely changed since the early ’80s. We can track its movements, prevent its spread, and use drugs to de-fang it once it’s in the body.
But a vaccine — that holy grail of medicine — has remained elusive. So far, at least.
All that might change, though. A new HIV vaccine trial, known as HVTN 702, has just started, supported in part by Fauci and the NIAID. It’s the most hopeful trial yet, based on an attempt from 2009 that lowered HIV infections rates by about 30%.
That first try was exciting, but it wasn’t quite good enough to distribute, so Fauci and his team are hoping that this new trial could be the kicker.
For the site of the drug trial, the scientists chose South Africa, a nation that’s been hit especially hard by HIV.
A Cape Town pharmacist checks documents on a fridge holding the vaccine. Photo by AP Photo/Schalk van Zuydam.
Fauci and the NIAID aren’t the only ones working on this. Dr. Gita Ramjee is the director of South African Medical Research Council’s HIV Prevention Research Unit. She’s been working on HIV prevention for years.
Ramjee explained that the location of the trial is significant. Worldwide, HIV/AIDS affects about 37 million people. 7 million of those cases are in South Africa. The country sees about 1,000 new infections every day, and women are especially at risk.
“In Southern Africa, the face of the epidemic is a woman’s face,” said Ramjee. That’s partly due to biological factors, but also social ones. Women don’t always have the power to negotiate condom use with their partner, for example, and there may be stigma around getting preventive care.
Ramjee is one of the scientists who has been trying hardest to help these women for years. She joined the vaccine push because she wanted to explore new ways to help people prevent infection and because she’s seen the costs of HIV/AIDS far too many times.
“Seeing these women in person, seeing a 16- or 18-year-old already coming to the clinic HIV-positive, it’s really, really heartbreaking,” said Ramjee.
That’s why it’s encouraging to see just how big this trial is. South Africa’s response recruited over 5,000 volunteers to take part.
One of the trial’s 5,400 volunteers at an event in Soshanguve, South Africa. Photo from Mujahid Safodien/AFP/Getty Images.
As part of this latest trial, South Africa enrolled 5,400 sexually active men and women. Half will get the vaccine, half will get a placebo. All will be offered established HIV prevention methods.
The trials will test the efficacy of the vaccine, and they’ll also test for any possible side effects. The first patient was enrolled on Oct. 26, 2016. Results are expected in late 2020.
Fauci and Ramjee aren’t making any predictions just yet, but both noted how huge an even moderate win could be.
Photo from Mujahid Safodien/AFP/Getty Images.
“Having a vaccine, even if it’s 50% efficacious, it’s going to add to the toolbox that we have,” said Ramjee.
Existing treatment and prevention methods such as condom use or vaginal rings have been able to take the edge off the infection rate, but they haven’t been able to completely reverse the disease’s trajectory. But immunization is a powerful tool, and added to our repertoire — well, that could be what finally tips the scales. It could be, as both Fauci and Ramjee said, the final nail in HIV’s coffin.
Yes, this trial could fail, but even if it doesn’t, it’s heartening to talk to folks who will keep going until one does. Research is, after all, a learning process.
“Irrespective of what the results are — positive or negative or moderate — we’re going to learn a lot,” Ramjee said.
That’s pretty cool. And on the cusp of this huge trial, it’s also worth celebrating just how far we’ve come since the virus first appeared.
Fauci still sees HIV patients in the very same room where he first met that first patient more than 30 years ago. He said the advancements in HIV/AIDS care he’s seen has been nothing short of breathtaking.
HIV/AIDS was once a death sentence. Today, with the right care, people can live long, happy, healthy, essentially normal lives. And we continue to see amazing strides in care, even now.
“It’s been a tremendous, extraordinary evolution,” he said.