7 mindblowing medical breakthroughs that could occur in our lifetime
One day soon, you might be able to grow new teeth. Seriously.
My family has a history of Parkinson's Disease, so I always see the headlines that promise some major scientific breakthrough in regards to the disease based on small, lab-based experiments or trials run on animals. They give us a glimmer of hope but, far too often, these treatments never see the light of day. The road from promising idea to having a real treatment available for patients is extremely long and arduous. Most potential new medications and therapies don't survive.
But... things do sometimes happen! There are massive medical breakthroughs being achieved all the time. Sometimes it's a new discovery, sometimes it's a successful clinical trial, and sometimes it's the fruit of all that labor finally becoming publicly available to people who need it the most. For example, an RSV vaccine just became available in 2023 for the first time. A powerful non-opioid pain killer was approved in 2024. A new drug came out to treat schizophrenia that was completely different than anything that had come before. Progress is being made every single year.
In our lifetime, say the next five to 20 years, we could see unbelievable advancements in treating certain medical conditions. Here are a few pretty amazing potential developments that are on the horizon.

1. Growing new teeth
Unlike sharks, humans are known to grow only two sets of teeth, our baby teeth and permanent adult teeth. If one gets knocked out or lost due to decay or infection, you're out of luck!
But researchers say growth buds exist in our gums for a third set, and scientists in Japan have had success in activating them to grow naturally. It could be a major gamechanger that could one day replace dentures and prosthetics. The team has moved onto human trials and has a target date of having a drug ready by 2030.
2. Cancer vaccines
Medical scientists have made amazing strides in cancer research, especially in the field of vaccines.
Did you know that lung cancer is considered to be the most deadly of the bunch? A lung cancer vaccine could be available very soon. If a cancer vaccine sounds odd, think of it this way: Cancer can be treated by chemotherapy and radiation, but there's always a chance of it coming back. People who have survived cancer could theoretically take the vaccine and massively improve their chances of reoccurrence.
A similar vaccine is showing promising results in clinical trials for pancreatic cancer.
3. Better treatment for Alzheimers
Alzheimer's Disease is one of the most destructive and heartbreaking conditions imaginable. It's also extremely difficult to treat, with most currently available therapies and medications focusing on slowing or temporarily relieving certain symptoms.
One new avenue scientists are exploring is a vaccine that could target a protein called tau, which clumps together and tangles up crucial neurofibers that deliver information in the brain. One such medication aims to activate a patient's immune system and produce "a strong antibody response against both pTau and its harmful aggregated form." The drug was recently fast-tracked by the FDA and has shown promising results in human clinical trials.
Another relatively new development is the availability of monoclonal antibody treatment, which helps slow the progression of the disease. Currently, the treatments are not particularly cost-effective but may become moreso in the near future.

4. Breakthrough treatment for Huntington's Disease
Huntington's is a fatal central nervous system disorder that shuts down key brain functions in patients like speech, walking, and cognitive function. Some of the symptoms can be treated but, so far, little can be done to slow or stop the progression of the disease.
However, a new drug known as PTC518 was recently fast-tracked by the FDA due to promising results in clinical trials. It attacks mutant Huntington protein in blood cells and in cerebrospinal fluid and has been shown to improve symptoms of the disease in a 12-month trial run. What's especially exciting is that this drug attacks the disease itself rather than just treating symptoms at the surface level.
5. Targeted viruses that kill antibiotic-resistant bacteria
Bacteria is getting smarter and evolving. Antimicrobial resistance is a grave threat to the global population as well-known antibiotics become less effective against infection and new antibiotics are expensive and difficult to develop.
(If you've ever dealt with a staph infection, you know how scary it is when drugs just... don't work.)
This is where special viruses, called bacteriophages or just phages, come into play. These viruses selectively target and kill bacteria, and were actually first used about 100 years ago. Scientist are coming around to using them again. In select settings, they've proven to be incredibly effective against resistant infections, but will need more testing before they become widely available. However, it's definitely possible that this become a viable alternative to antibiotics in some cases in the next few decades!
6. Synthetic and bioprinted organs
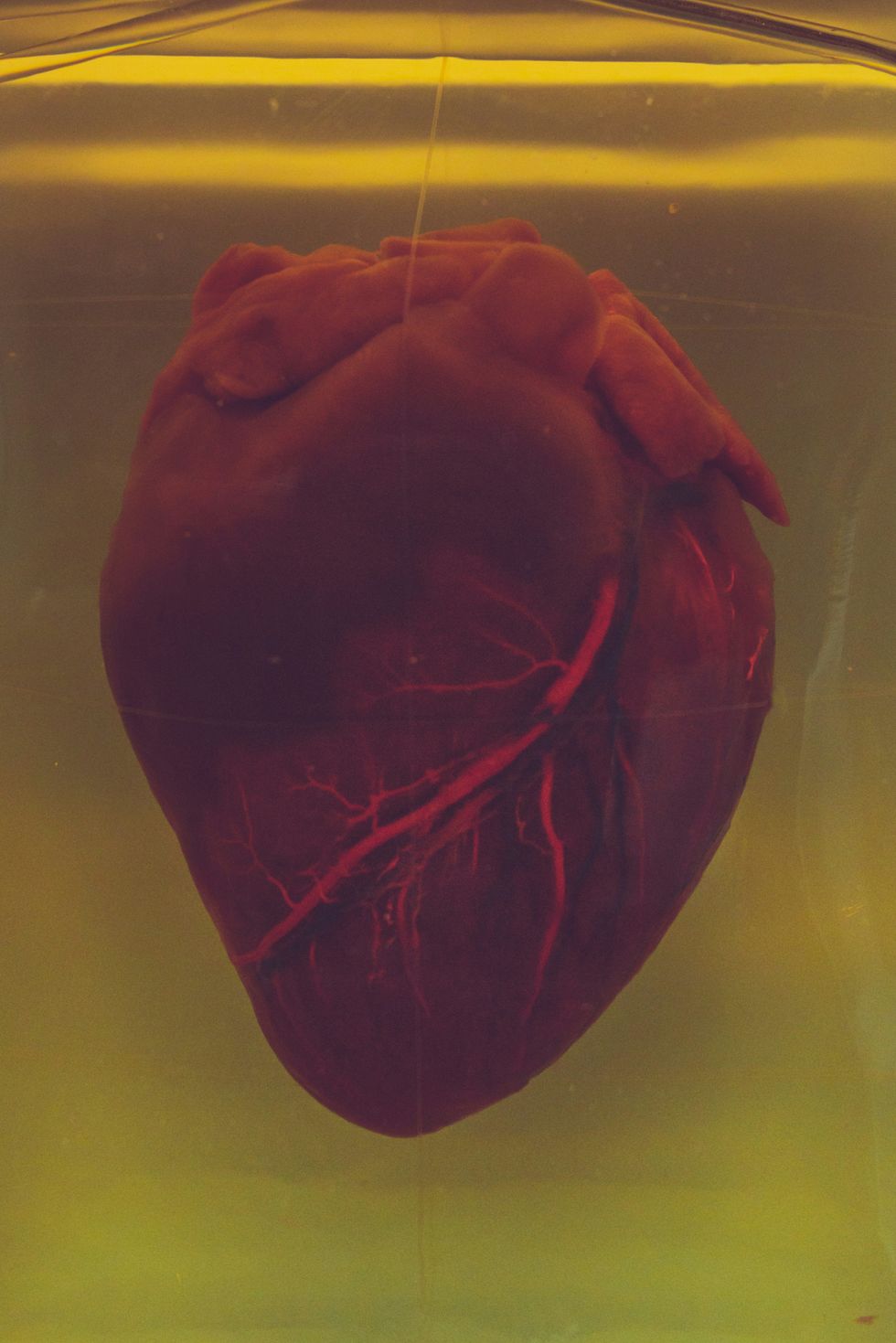
There are simply not enough donor organs going around for all the people who need a healthy liver, heart, or kidney.
Luckily, incredible strides have been made in creating artificial organs that can function like the real thing. A man in Australia just lived for 100 days with a titanium heart while he awaited a transplant! And bioprinting technology – quite literally 3D printing using real tissue and living cells — has the potential to create new working organs from scratch in the near future. Genetically modifying animal organs to function in humans temporarily or maybe even permanently has also come an extremely long way and is a process that will drastically improve in the coming years.
7. A one-pill cure for Hepatitis B
Hepatitis B is a potentially fatal infection of the liver that affects hundreds of millions of people worldwide. There is a safe and effective vaccine available to some people, but it's only preventative and won't treat active infections.
A research team in Israel recently discovered that a low dose of well-known chemotherapy drug, Curaxin-137, completely destroyed a crucial and mysterious protein that the Hepatitis virus depends on. The testing was done in a lab setting, so the next step is clinical trials. The team hopes that one day in the not-so-distant future, patients could take a single dose and completely eradicate the virus in their system. That's about as close to a miracle-cure as you can get!
Not all of these potential breakthroughs will come to fruition, but it's pretty amazing to dig into the advancements and discoveries that are being made every day. This list is just scratching the surface, to say nothing of robotic surgeons that will make major surgeries less invasive, new treatments for baldness, nanotechnologies that can deliver medicine to specific parts of the body, and more. Ultimately, good news is coming relatively soon for people who need it.
