A few years ago, there was an online trend in which Americans posted things the “European mind can’t comprehend,” a series of memes featuring photos of vast spaces, incredibly huge restaurant portions, and Costco shopping sprees, to name a few. It was basically a joke about American grandiosity, which contrasts with more modest European sensibilities.
A significant difference between the European Union and the United States is size. Europe comprises 47 countries spread across 3,837,083 square miles, and the United States is one country covering 3,796,742 square miles. Therefore, in the U.S., the distance between major cities, especially in the west, is hundreds, if not thousands, of miles. Europeans may casually think that the U.S. is the size of a single country, such as Germany, when in reality, each state is the size of a European country.
The difference in distance and size leads to some rather funny moments in which Europeans assume they can travel from one coast to another in the same day. Or, at least, to different destinations in the same state in an hour or two. However, this couldn’t be further from the truth.
A Reddit user on the Casual Conversations subforum shared a funny story about a friend from the UK who thought they could wake up in Los Angeles, drive to the Grand Canyon for a quick hike, and then have dinner back in West Hollywood. In reality, even on a weekend, this round trip would take about 17 hours in the best-case scenario. That's without factoring in time to hike the canyon. The story inspired other Americans to share funny stories about friends in Europe who seriously underestimated the size of the U.S.
 A tourist takes out their map.via Canva/Photos
A tourist takes out their map.via Canva/Photos
Here are 11 funny stories about Europeans who misjudged the size of the U.S.
1. Detroit for the afternoon?
"Not me, but my grandparents. They'd emigrated from Germany to the US in the late 1920's while in their 20s. Lived in the NY metro area. Somewhere in the 1960 or 70s or so, they had friends or relatives (I don't remember which) visiting from the old country who asked if they could perhaps drive to visit other friends of theirs, maybe for afternoon coffee one day... in Detroit. They politely explained that wouldnt work and how far it was.... but chuckled about it for decades after the visit."
"Detroit for coffee?! That is a 600-mile latte run."
2. Stop by Seattle?
"Distant relative from Austria was visiting his friend in Connecticut. Asked if he could stop by and see me on his week-long trip. I live in Seattle."
3. Stop by Dallas for dinner?
"My mom speaks Italian and on her way home one year, her plane was about to land in Chicago when she heard the two Italian men behind her excitedly talking about their plans. One said to the other, 'Okay. We'll pick up the rental car and then we'll drive to Dallas for dinner.' My mom eventually got them to realize that they'd be spending two full days in the car just getting to Dallas if all they did was drive. She suggested they find some food in Chicago instead."
 The freeway leading into Dallas.via Canva/Photos
The freeway leading into Dallas.via Canva/Photos
4. Shopping in San Francisco?
"My uncle is from Hawaii. He thought we could drive from LA to San Francisco to shop that morning and then maybe hit Venice Beach before dinner."
5. San Francisco for dinner?
"Fellow Angeleno here. When I was still in my last retail job, we got a lot of overseas tourists, and it wasn’t unusual for them to not realize how BIG the USA is. One customer asked me 'We’re thinking about going to San Francisco for dinner. What time should we leave?' He was so shocked when I explained that San Francisco was about an 8-hour drive with afternoon traffic."
It is about 380 miles to get from Los Angeles to San Francisco.
6. LA, DC, Miami in a single day?
"I had a group of EU friends who wanted to visit the US for a week. By the time I got out of that 5hr group call, they cancelled the whole trip. They wanted to land in Seattle, spend about 3 hours with me giving them a tour of the city, get a rental car, and explore LA, DC, and Miami all in a single day. The next day, hit up Yellowstone, the Grand Canyon, and mt rainer. The day after, hit up a Buckees for breakfast in Texas, eat lunch in NYC, and have dinner at my place in Seattle with my family, then go to Las Vegas after dinner to go party... Oh, and they only had $500 each (2k total), with plans to individually pay their own way, no travel insurance, and no temporary "travel" phone plans (meaning no phone service OR insured hospital visits if something went wrong). First thing i did when i got added to the call was pull up a pic of the US overlayed on top of Europe, and pointed out where seattle was, and all the other places they wanted to go, in comparison to Europe. Instantly deflated in excitement, then i went into cost of living for each state they wanted to visit."
7. 9/11 worries
"A Scottish family we knew lived in the States during 9/11. They got several concerned calls from friends and family wanting to make sure if they were okay and asking if they could see the Towers. They were in Michigan."
8. Why American's 'don't travel'
"I think this misunderstanding is at the root of a lot of how Europeans can judge Americans for “not traveling.” If it takes someone two hours to get to a different country and it takes me more than two hours to drive across Massachusetts, then the cost and time burdens aren’t equivalent."
9. How close is Florida to California?
"I was in Belfast earlier this year. The woman at the hotel front desk asked how the 'long drive' from Dublin was. As Americans, we were like, Oh, it wasn’t bad at all. Everything is a long drive in America. And she said, 'Yeah, it’s probably like twelve hours from Florida to Cali.'"
In reality, it would take about 45 hours to drive from San Francisco to Miami.
10. Walk from Syracuse to NYC?
"Years ago, a friend in the former Czechia was thinking of going to art school in NY. They were excited that they would be able to study, and have fun in the NYC clubs at night. The school was in Syracuse. It broke both his heart and brain when I told him it would be a 4.5-hour drive to NYC. He was under the impression he could 'just walk there.'"
11. Disney to Disney in 6 hours?
"Had a friend who wanted to rent a car and drive from Disneyland to Disney World. When they told me I immediately started laughing.They had no idea of how big the USA is and thought it might be a 6-hour drive tops."
In reality, it would take around 40 hours to drive from Disneyland in Anaheim, California, to Disney World in Orlando, Florida.


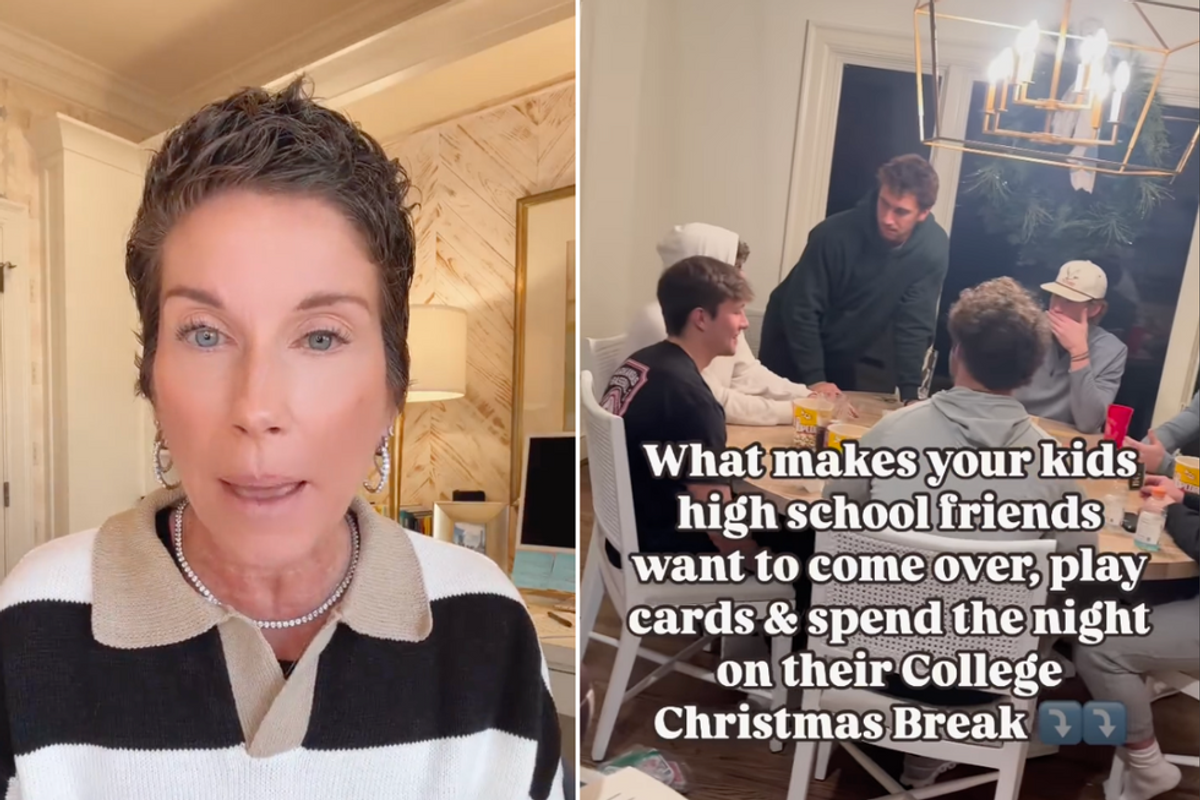
 Teens hanging out in a living room.via
Teens hanging out in a living room.via  Teenagers eating pizza.via
Teenagers eating pizza.via  Teenagers eating pizza.via
Teenagers eating pizza.via 
 Three inhales is all it takes.
Three inhales is all it takes. Spicy foods can trigger hiccups.
Spicy foods can trigger hiccups.
 Student smiling in a classroom, working on a laptop.
Student smiling in a classroom, working on a laptop. Students focused and ready to learn in the classroom.
Students focused and ready to learn in the classroom.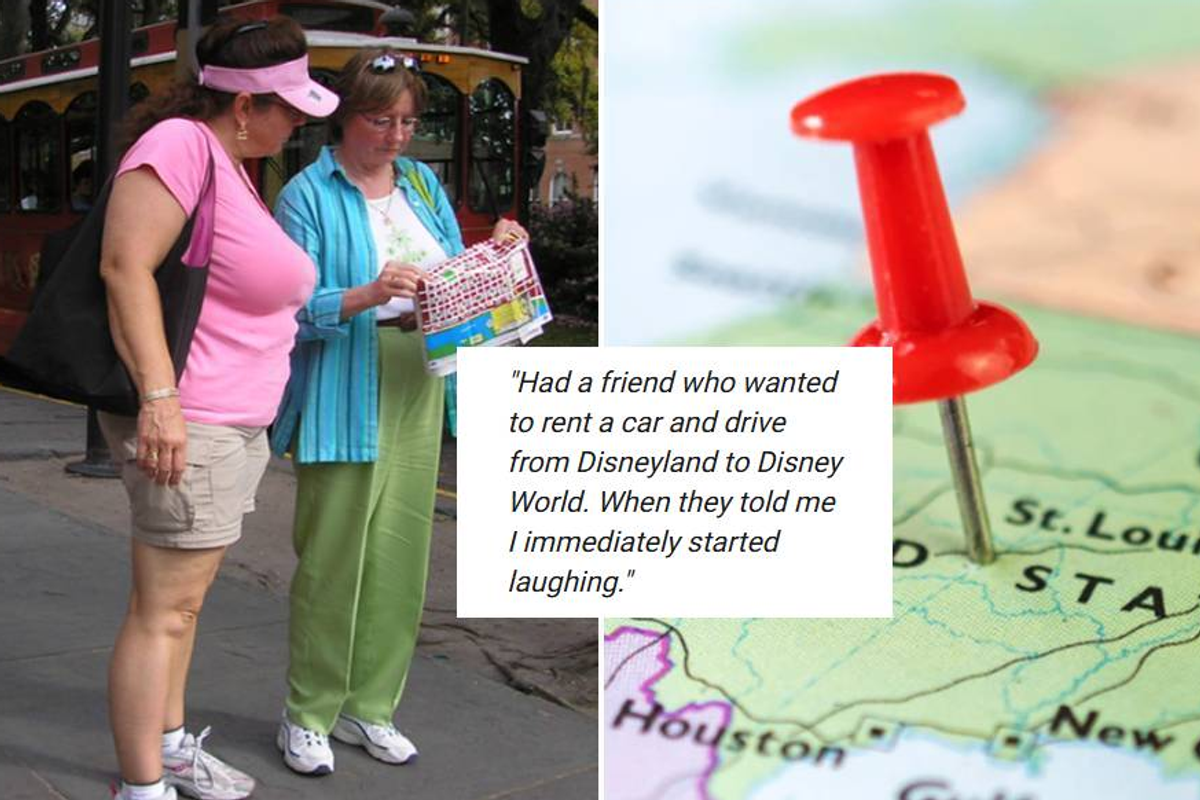
 A tourist takes out their
A tourist takes out their  The freeway leading into Dallas.via
The freeway leading into Dallas.via 