On March 26, 2022, as the final seconds ticked away from Genesis’ farewell tour, the crowd at London’s O2 Arena was clearly emotional. The prog-pop band’s most famous lineup—front man Phil Collins, guitarist/bassist Mike Rutherford, and keyboardist Tony Banks—had finally reunited after a 13-year hiatus (and a temporary pandemic delay), and no one wanted this improbable run to end. But there may have been another reason for the sadness: a glaring absence onstage.
Peter Gabriel had co-founded the band in 1967, helping catapult them to rock glory with his golden rasp and surreal stage antics, before leaving in 1975 to launch a solo career. Collins, previously the drummer, got the promotion to lead singer, leading the group through the commercial heights of “Mama” and “Invisible Touch.” Hardcore prog fans pined to hear Gabriel sing Genesis again, but outside of a few powerful one-offs—a tease of their epic “Dancing With the Moonlit Knight” during a 2016 solo tour, a 1999 re-recording of their starry-eyed ballad “The Carpet Crawlers”—that door remained shut.
- YouTube www.youtube.com
Now here he was at the O2, seated among the commoners, with an opportunity to help bring the Genesis story full-circle. Instead, he took the unselfish (if, let’s face it, slightly unsatisfying) route: avoiding the spotlight and letting his former bandmates enjoy the curtain call they’d rightly earned. (“Me going was a rite of passage, really,” the singer told Mojo in 2023. “I’d been part of the creation of Genesis, so I wanted to be there at the end.”)
Here’s the thing, though: A lot of casual fans forget that Gabriel had already reunited with Genesis for an entire show—it just happened 20 years earlier. Oh, and it occurred not because of rosy nostalgia but due to mounting debt and death threats.
The reunion stemmed from the financial disaster of the first WOMAD
Gabriel staged the inaugural WOMAD (World of Music, Arts, and Dance) in July 1982, with the noble vision of sparking genuine cultural fusion. The three-day event featured British post-punk (Echo and the Bunnymen, Pigbag) and art-rock (Peter Hammill, Robert Fripp), traditional Irish folk (The Chieftains), Indian sitar players (Imrat Khan), Afro-Caribbean dance companies (Ekomé)—a legit anything-goes atmosphere that remains novel at music festivals decades later, let alone in the early days of MTV. "I [wanted] to celebrate all these fantastic musicians, art, dance, film from around the world that weren't getting exposure,” Gabriel told filmmaker John Edginton in a raw-footage clip filmed for his 2014 documentary, Genesis: Together and Apart. He had big dreams for WOMAD, and, as he noted in the 2007 book Genesis: Chapter and Verse, the first fest was “magnificent.”
- YouTube www.youtube.com
"We put it on during school time, so there were a lot of schools working on projects about world music; it was very exciting, fresh, passionate,” he said. “But the people just didn’t come. There was a rail strike that weekend, and even though we thought we had enough names to pull in an audience, we were hopelessly under each day, and suddenly realized the financial consequences.”
Gabriel found himself in an alarming situation, receiving “horrible phone calls and death threats” from his creditors. “It was a very oppressive nightmare,” he said. Luckily, his old band stepped in—not that anyone involved would have chosen the reunion without this dire prompt.
By 1982, Gabriel had been enjoying a successful solo career, crafting artful pop songs and studio experiments while tinkering with new recording technology (the Fairlight CMI sampling synthesizer, for one). He had little interest in looking backward—outside of a couple early solo tours where he was forced to play a Genesis song or two due to a lack of material, he’d more or less distanced himself from his old band. (His debut single, “Solsbury Hill,” is about his desire to leave Genesis—and the music business entirely. “I felt like I was just in the machinery,” he told Rolling Stone, citing a lyric. “We knew what we were going to be doing in 18 months or two years ahead. I just did not enjoy that.”) The band, meanwhile, had soldiered on just fine without their original front man, growing into a stadium act with Collins behind the mic.
- YouTube www.youtube.com
"It made sense to us"
When manager Tony Smith reached out to Genesis, seeing if they could help Gabriel escape his dark spiral with a one-off benefit reunion, everyone felt it was the right thing to do. “Whether or not he felt he needed our help to get himself out of trouble, it made sense to us,” Collins wrote in Chapter and Verse, “and it certainly was not a condescending gesture.” Banks added that, beyond the kind act of helping their friend, it made sense as an act of fan service: “People had been asking us to organize some sort of get-together for years and years, and this seemed a very good reason to do it, at the same time as helping Peter pay off this particular debt. We did need a reason because it wasn’t something we were itching to do."
It’s not like they hated each other: Collins had even played on Gabriel’s self-titled 1980 solo album, helping create the distinctive “gated” drum sound that became ubiquitous throughout the decade. But it was a somewhat awkward fit musically, given how far their respective sounds had diverged. "Having tried for seven years to get away from the image of being ex-Genesis, there's obviously a certain amount of stepping back," Gabriel reportedly told NME ahead of the show. "I don't think they would choose at this point to work with me … [but] I’m very grateful and I'm intending to enjoy myself."
- YouTube www.youtube.com
The problem was how to solve their logistical puzzle—Genesis was only still playing a few of their Gabriel-era songs, and their old front man wasn’t up to speed on any of them. They managed to arrange two or three rehearsals at London’s Hammersmith Odeon, where Genesis played a triple-header on September 28th, 29th, and 30th. The quirky set drew from Gabriel’s time in the lineup, sprinkling in one solo cut (“Solsbury Hill,” ironically) and a single '80s-era track (“Turn It on Again,” with Gabriel on second drums). Understandably, the performances were rather loose—not up to anyone’s respective standards—and the massive downpour of rain probably didn’t improve anyone’s mood.
But in the widely shared bootlegs of that show, fans were just happy to see everyone on stage again. They even saw a brief reunion of the full ‘70s quintet lineup: Former guitarist Steve Hackett, who learned about the event while on vacation in Brazil, flew back to the U.K. to play on “I Know What I Like (In Your Wardrobe)” and “The Knife.” "As they’d already rehearsed up their stuff, I was only able to join the encores,” he wrote in his 2020 book, A Genesis in My Bed, “but I was thrilled to be involved with the team once more."
- YouTube www.youtube.com
“It felt like a bit of a dream”
It’s easy to look back on the gig with a what-if feeling. Could they have somehow figured out more rehearsal time? (Probably not.) Should they have professionally recorded the event, no matter how sloppy they expected it to be? (Definitely.) “I regret it now, but I was keen not to record the show,” Rutherford wrote in his 2015 memoir, The Living Years. “I thought it would be a bit rough and ready and that it was better to be there and in the moment.”
Ultimately, what matters is that with Six of the Best, Genesis accomplished their primary goal: rescuing their old friend from a terrifying plight.
“It felt like a bit of a dream,” Banks wrote in Chapter and Verse. “I was very glad when it was over, because I hadn’t particularly enjoyed playing that stuff at the time. I always tended to be into what we were doing either at the time or whatever the next thing was. I was pretty glad to have left some of those old songs behind. But the audience reaction was very good, and I believe that show did go some way to sorting out Peter’s financial problem; now WOMAD is a monster thing.”
Indeed. The festival re-emerged stronger in the mid-’80s and has continued annually—without death threats—ever since.
Gabriel might have been watching the final Genesis show, but he was on stage in spirit. Collins gave him a shout-out during the set, and the band wrapped this historic occasion with their swirling ballad “The Carpet Crawlers,” a track Gabriel helped craft for his Genesis swan song, 1974’s The Lamb Lies Down on Broadway.
Few major rock bands have replaced one iconic singer with another. Even fewer have done it by promoting from within. And while Genesis achieved such longevity because of their songwriting—the imagination, the color, the dynamics—perhaps that familial spirit had something to do with it. They weren’t always on the same page, musically or otherwise—but as Six of the Best proved, they came through for each other when it mattered most.
- YouTube www.youtube.com



 In a 4-day model, kids often (but not always) receive less instructional time. Photo by
In a 4-day model, kids often (but not always) receive less instructional time. Photo by 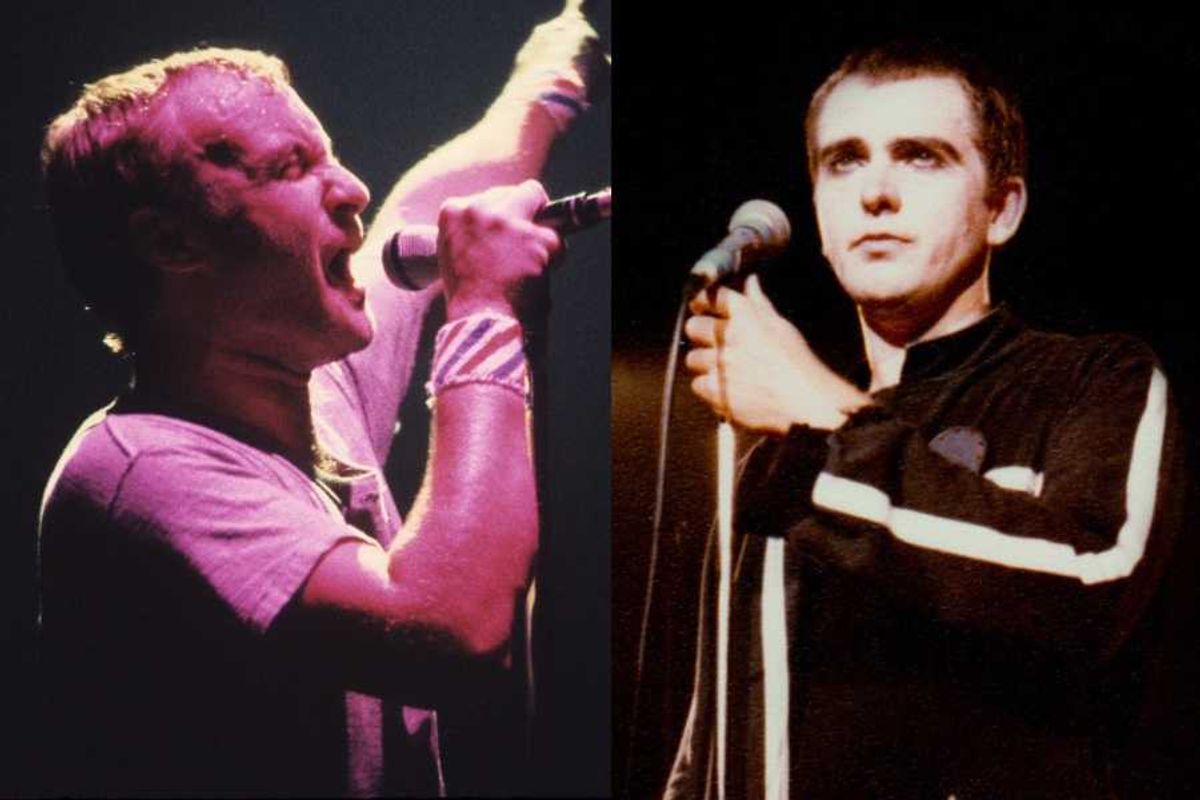

 Two woman having a heart-to-heart conversation. via
Two woman having a heart-to-heart conversation. via  A man who has dug in his heels. via
A man who has dug in his heels. via