Tipping has been standard practice in the United States for over a century.
But why don’t we just pay it all in one bill? Let’s start at the beginning.
Photo by Nan Palmero/Flickr.
Tipping was started in the 17th century by British aristocrats as what journalist Paul Watcher describes as “a sprinkle of change for social inferiors.” It was brought to the U.S. by rich Americans who vacationed in Europe after the Civil War.
When the practice arrived, people weren’t that into it — it was viewed as un-American. Despite that, it stuck with us, and today about 4.3 million people make a living mostly on tips.
How did tipping go from being just a little something extra to a full-on means to an end?
The big change came in 1966, when the Fair Labor Standards Act was amended with a subminimum wage for tipped workers and a tip credit for employers.
Through tip credits, employers of tipped workers are being subsidized by consumers at record levels. Chart by Economic Policy Institute.
That change allowed employers of tipped workers to offload the responsibility of paying the legal federal minimum wage onto their customers.
The current federal minimum for tipped workers (those earning more than $30 per month in tips) of $2.13 an hour hasn’t budged since 1991, when the inflation-adjusted value of the dollar was 75% higher than it is today. By comparison, the federal minimum wage has been increased six times in the same period.
There’s a growing trend in the service industry to toss the tipping system.
One of the latest to join is famed New York restaurateur Danny Meyer, who you may know better as the founder of Shake Shack.
Shake Shack gained national fame after creating burger and fries recipes that turned everyone within a three block radius of their exhaust fan into a beef-craving zombie. This is the original Shake Shack in Madison Square Park, New York City. Photo by Lucius Kwak/Flickr.
Meyer is eliminating the traditional tipping system by building a service charge (and then some) into the prices at all of his full-service restaurants. He wrote on his company website that tipping was getting in the way of their ability to provide “meaningful career opportunities and advancement” for their 1,800 employees.
According to New York Eater, Meyer has been talking about it for decades. In a 1994 newsletter, he explained his qualms with the practice of tipping:
“The American system of tipping is awkward for all parties involved: restaurant patrons are expected to have the expertise to motivate and properly remunerate service professionals; servers are expected to please up to 1,000 different employers (for most of us, one boss is enough!); and restaurateurs surrender their use of compensation as an appropriate tool to reward merit and promote excellence.”
All-inclusive pricing could make tipping a thing of the past.
Not all tipped workers struggle under the current system, but most of them aren’t servers in fancy restaurants with the guarantee of 20% commissions on every sale. Meyer wants the shift away from tipping to “right what has been a labor of wrong.”
“Tipping is awkward,” says Danny Meyer. Photo by Nicholas Kamm/AFP/Getty Images.
The restaurants will not only take responsibility for fairly compensating their servers, but the price hikes are also going to lift the bottomed-out wages of non-tipped employees, like front-of-the-house staff, cooks, and even entry-level managers.
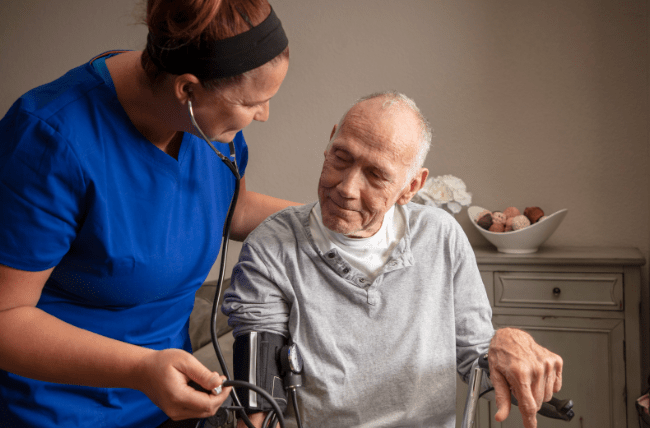
Photo via iStock.
This could be the start of a new era of humane hospitality.
Meyer is giving the no-tips model some important visibility and traction, but small businesses around the country beat him to implementing all-inclusive pricing.
One of those businesses is Lanesplitter, my go-to pizza joint here in Oakland. They call it a “sustainably served” model. Their employees earn living wages and have access to paid time off, health care, and overtime pay — things all workers deserve.
Sure, ditching the tip might feel like a big change, but when you consider all the downsides, it’s hard to argue against it. Thankfully, it looks like more people are beginning to recognize that.